Brain cells gone haywire during sleep may lead to chronic pain, mouse study suggests
A mouse study hints at why chronic pain and poor sleep are linked.

Scientists may finally have an explanation for why poor sleep is tied to chronic pain. A new mouse study suggests that nerve injuries make certain brain cells go haywire during sleep, and this sudden excitement may lead to chronic pain. Conversely, stopping the hyperactivity during sleep can help relieve the pain, the study hints.
People with chronic pain often experience sleep disorders, including insomnia, and evidence suggests that poor sleep quality is a major risk factor for developing chronic pain in the first place. Although this link is well-established, "the nature of the sleep problems for different pain conditions, their precise causes or their long-term consequences are yet unknown," said Alban Latremoliere, an assistant professor of neurosurgery and neuroscience at the Johns Hopkins School of Medicine, who was not involved in the new study.
"You will often hear about the 'vicious circle' whereby pain disrupts sleep, which in turn worsens pain, but the biological pathways involved have been extremely elusive," Latremoliere told Live Science in an email. The mouse study, published Monday (Jan. 23) in the journal Nature Neuroscience, starts to unravel the inner workings of one of these mysterious pathways, he said.
The study focused on neuropathic pain, which arises from an injury or disease in the nerves that relay sensory information from the body to the brain. The researchers studied mice with injuries in one of the sciatic nerves, the major nerves that extend from the spinal cord to the hind legs. Two of the nerve's three branches that plug into the leg were injured, and this caused the skin supplied by the remaining branch to become hypersensitive, explained Guang Yang, senior author of the study and an associate professor of anesthesiological sciences at the Columbia University Irving Medical Center in New York City.
Related: Can you make up for lost sleep?
"It mimics human neuropathic pain related to peripheral nerve injury," Yang told Live Science in an email.
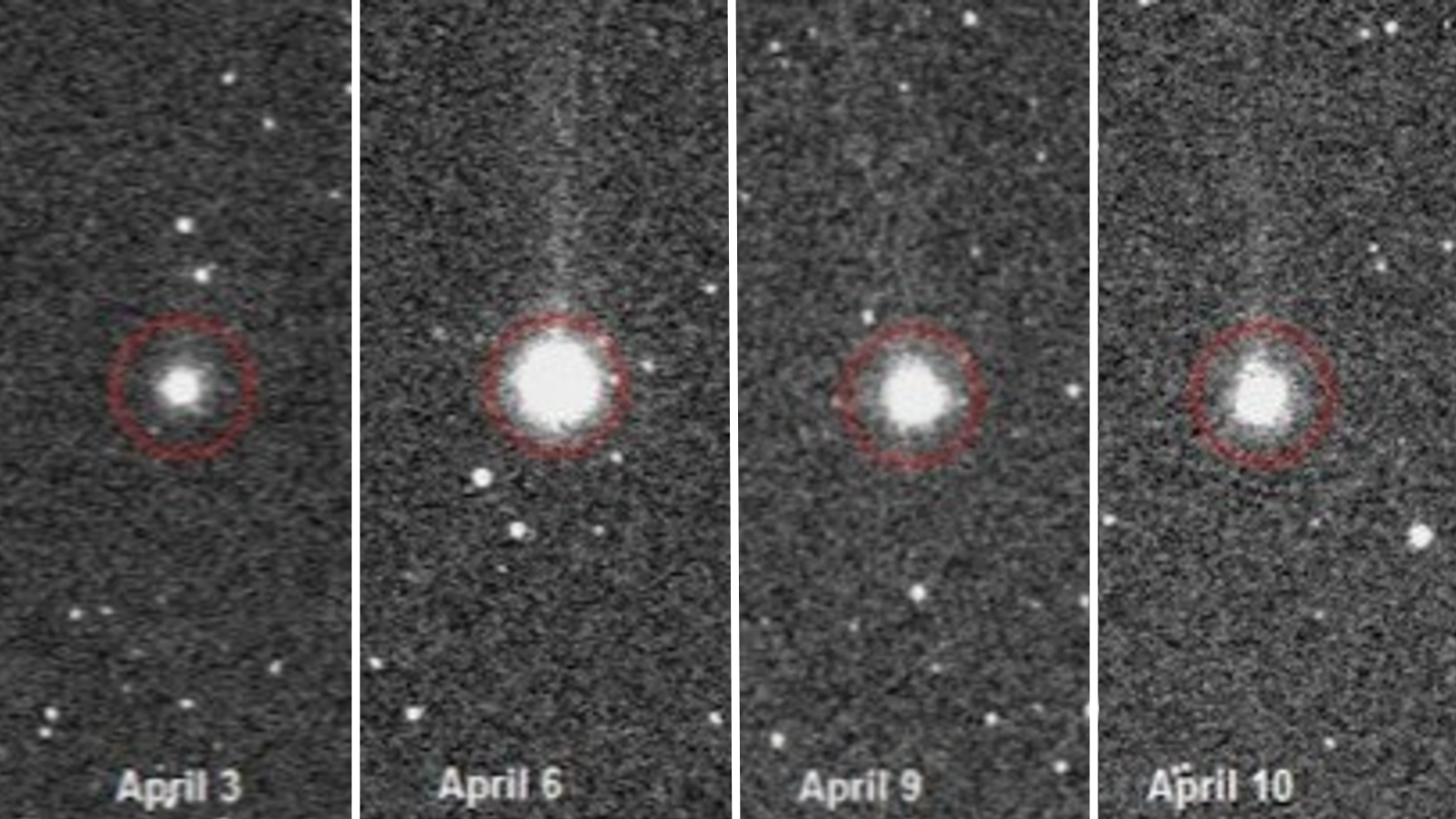
The team analyzed the rodents' brain activity before and after injury and spotted distinct changes in the region of the wrinkled cerebral cortex that receives sensory data from the hind leg. Brain cells with pyramid-shaped bodies, aptly named pyramidal neurons, became progressively more active in the weeks after injury, as the mice's pain entered the chronic phase. But their hyperactivity peaked during non-rapid eye movement sleep (NREM), when deep sleep occurs.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Why did these pyramidal neurons go haywire? The team traced the blame back to the anterior nucleus basalis, a cluster of neurons lodged deep in the front of the brain.
The activity of this cell cluster had also increased after injury, the team found, and this led the cells to send the chemical messenger acetylcholine up to the cerebral cortex. Through a chain reaction, this action essentially lifted the breaks off the pyramidal neurons, shifting them into overdrive.
This shift in brain activity was linked to a change in pain sensitivity in the mice, where once-painless stimuli suddenly became painful. In a series of experiments, the researchers found that they could relieve this pain by blocking the hyperactivity of different cells in the brain pathway they'd discovered.
"Inhibition of this pathway during NREM sleep, but not wakefulness, corrects neuronal hyperactivation and alleviates pain," the researchers wrote in the study.
Eventually, this line of research could lead to new treatments for humans with chronic pain, but this initial study is somewhat limited because it's in mice.
"While I believe the same problems observed in mice are likely to occur in humans, their exact profile and distribution might vary in patients," partially because humans' circadian rhythms differ from those of the nocturnal rodents, Latremoliere said. He added that he'd be interested in seeing whether this newfound pathway contributes to other types of chronic pain, such as cancer- or chemotherapy-related pain.
Yang and her colleagues aim to study whether their results carry over to humans. The current study raises the idea that chronic pain may be "encoded" in the brain during sleep, not unlike how memories are built into the brain during sleep, she told Live Science.
"The knowledge that neural circuit remodeling during sleep plays such a vital role in the formation of chronic pain is highly relevant to pain therapeutics," she said.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.