Can CBD really prevent COVID-19 infection? Scientists hope to find out.
Research suggests marijuana ingredient could block the coronavirus.

Cannabidiol (CBD), an active ingredient in cannabis, might help block infection with the virus that causes COVID-19.
But don't go drop a bunch of cash on CBD oils at your local dispensary: The possible effect still needs to be tested in humans. (And definitely don't smoke marijuana to prevent coronavirus infection.) Even if the findings do hold up, they apply to the kind of medical-grade, Food and Drug Administration (FDA)-approved CBD used to treat seizure disorders, not the low-potency stuff available to consumers.
CBD is also no substitute for weapons against COVID-19 that are known to work, such as vaccination and high-quality masks, said study leader Marsha Rosner, a cancer researcher at the University of Chicago who studies immune responses. But the researchers are hopeful that the compound could be an additional tool in the fight against the SARS-CoV-2 virus — and perhaps other viruses. So far, the team has shown that the compound can help mice fight off COVID-19, and they've turned up suggestive evidence that it might be helping humans, too.
"We don't know yet if CBD can prevent COVID, but we think our results provide a strong case for conducting a clinical trial," Rosner told Live Science. "That's really our mantra: We want a clinical trial."
Triggering stress
CBD is derived from the cannabis plant. Unlike tetrahydrocannabinol (THC), the main psychoactive ingredient in marijuana, CBD doesn't cause a high. But it does bind to more than a thousand different receptors in the human body, said Robin Duncan, a biochemist and nutritional scientist at the University of Waterloo in Ontario, who was not involved in the new research. This biological activity has given it a reputation as a health supplement — CBD oils, shakes and other products are available all over the place — but little about CBD's impact on health has been tested or proven.
Rosner and her colleagues stumbled into studying CBD and COVID-19. They were screening compounds for cancer research, trying to trigger an immune response in cells called the host stress response. The host stress response is part of the innate immune response. It's not targeted at any particular pathogen, but when a cell senses a threat, such as an invading virus, this response puts the cell into a defensive state, triggering the release of protective chemicals and helping prevent the cell's machinery from being used to replicate the virus.
"Smoking or vaping pot won't protect you against COVID-19."
—Marsha Rosner
CBD seemed surprisingly good at triggering the host stress response, which is important for cells to fight back against viruses, Rosner said, so she and her colleagues decided to study the compound against the novel coronavirus.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
They began by treating human lung cells in a lab dish with CBD and then exposing them to SARS-CoV-2, the virus that causes COVID-19. They found that compared with untreated cells, the CBD-dosed cells were much better at staving off infection. The same held true for monkey kidney cells, which are susceptible to the virus. It also held true for the alpha, beta and gamma variants of the coronavirus. (Delta and omicron weren't available when the study was done, Rosner said.)
"We show that CBD can stop replication of SARS-COV2 in cells in a dish and that it acts at least up to 15 hours after infection, so that suggests it might be effective even at early times after viruses enter cells," Rosner said.
Putting CBD to the test
Cells in a dish are one thing; living organisms are another. The researchers next tested the compound in mice, injecting pure CBD into the guts of the animals daily for seven days and then spraying live SARS-CoV-2 into their nasal passages — a surefire route to infection. They then continued the CBD injections for four more days.
Five days after the viral treatment, the researchers measured the viral load in the nasal passages and lungs of the mice. They found that with a low dose of CBD, the viral load was 4.8 times lower in the lungs and 3.7 times lower in the nasal passages compared with untreated mice. With a high dose, the viral load in CBD-treated mice was 4.8 times lower in the nose and a whopping 40 times lower in the lungs than in untreated mice. The infected mice also seemed to be fighting off the pathogen with relative ease: Lab-infected mice typically become ill and lose weight, but the CBD-treated mice showed no symptoms.
CBD is an FDA-approved treatment for some seizure disorders, so some people take regular oral doses of the pure compound, Rosner said. She and her team combed through the medical records of people with seizure disorders, comparing the rates of COVID cases in those taking CBD as a treatment to those with similar demographics and medical histories who weren't using CBD, about 530 in each group. They found that the rate of COVID-positivity in those actively taking CBD was 4.9%, compared with 9% among those not taking it.(However, because it was based on medical records alone, the study couldn't rule out that there might be some unknown differences between the two groups that might independently affect their risk of COVID exposure.)
An immune booster?
With these promising findings in hand, the team then turned to investigating other cannabis compounds, such as cannabidiolic acid (CBDA), cannabidivarin (CBDV), and THC. They found that CBD alone demonstrated antiviral action. In fact, combining CBD with THC, as one might find in recreational marijuana products, reduced CBD's antiviral effect. In other words, smoking or vaping pot won't protect you against COVID-19, Rosner and her colleagues wrote in their new study, which was published Jan. 20 in the journal Science Advances. In fact, smoking or vaping might cause lung damage that can put a person at more risk if they do catch the disease.
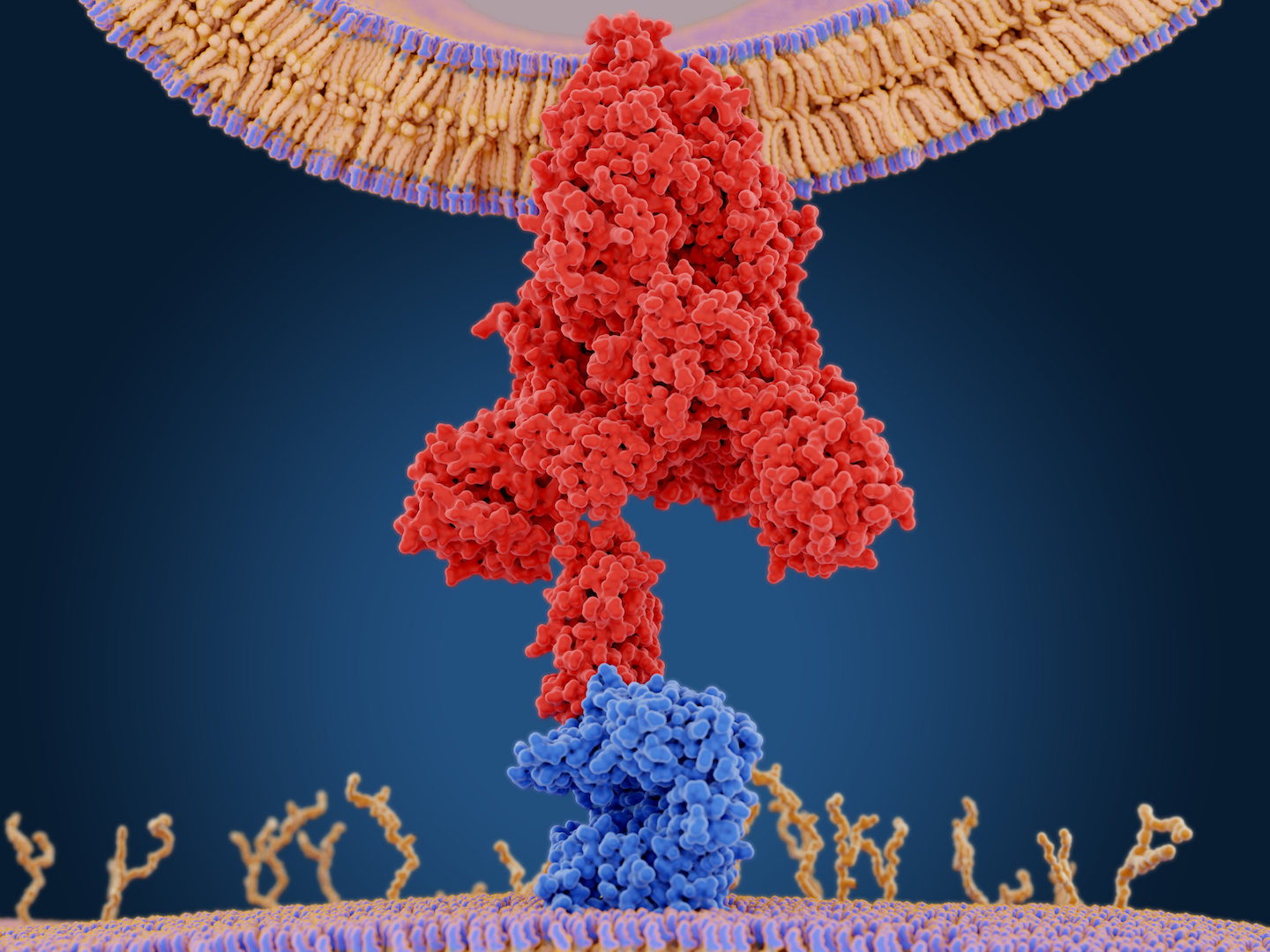
The team also investigated why CBD might be having an effect. They found that CBD activates a couple of different protective processes in infected cells. One, known as the "unfolded protein response," works on the cell machinery that gets hijacked by the virus to make more copies of itself; this response helps maintain function in a cell that is under stress. The unfolded protein response is so named because it helps halt the cell's production of proteins and clear misfolded or unfolded proteins that are gumming up the works. CBD also helped trigger the production of interferons, immune system compounds that mount a first-line defense against viral replication within the cell.
The SARS-CoV-2 virus has its own defenses that help it suppress a cell's interferon production; some early research hints that the omicron variant is less severe than previous variants because it doesn't suppress its host's interferon production as much. If CBD is capable of boosting interferon even as the virus tries to suppress it, CBD might help reduce disease severity.
Similar results have been seen in other labs, including Duncan's. Duncan and her colleagues have studied the effect of CBD on specific genes within SARS-CoV-2 infected cells and found results that complement Rosner's. In that research, which has not yet been peer-reviewed but has been posted on the preprint database bioRxiv, Duncan and her team found that kidney cells infected with SARS-CoV-2 did a poor job of mounting a frontline antiviral defense. But cells treated with CBD and infected showed a marked increase in genes involved in antiviral action.
"Overall, we both saw similar things: us, when we were looking at specific genes; and them, when they were looking at the whole virus," Duncan said.
In another recent study published in the Journal of Natural Products, researchers at Oregon State University reported that cannabigerolic acid (CBGA) and cannabidiolic acid (CBDA) could bind to the coronavirus spike protein and prevent the virus from entering cells. That's a different mechanism of action than shown in Rosner or Duncan's research, as well as different cannabis compounds. That study also focused solely on cells in a petri dish, not in animals or humans. It's not yet clear whether the CBGA or CBDA used in that study could be metabolized effectively to work in a living organism, Rosner said. CBD metabolism is better understood from its use in seizure treatment.
To apply for clinical trials in humans, scientists have to show preclinical data suggesting that a drug might have an impact and must also show evidence of safety. Rosner and her team have provided that preclinical data, Duncan said, and CBD is already well-known to be safe and nontoxic in most people. The FDA-grade compound is approved for the treatment of seizures in anyone over the age of 1 in the United States.
A study testing whether CBD could prevent infection would require a huge sample size, on the scale of the studies used to prove the efficacy of vaccination, Rosner said. For that reason, it's more likely that the researchers will first launch a clinical trial testing whether CBD could help reduce symptoms or severity if taken right after COVID infection. They hope to move forward with those trials in the near future.
"We need to find a sponsor and we need to find funding, so we've been in conversation with both companies and our government about how to do that most effectively," Rosner said.
Originally published on Live Science.

Stephanie Pappas is a contributing writer for Live Science, covering topics ranging from geoscience to archaeology to the human brain and behavior. She was previously a senior writer for Live Science but is now a freelancer based in Denver, Colorado, and regularly contributes to Scientific American and The Monitor, the monthly magazine of the American Psychological Association. Stephanie received a bachelor's degree in psychology from the University of South Carolina and a graduate certificate in science communication from the University of California, Santa Cruz.