The sneaky way the coronavirus mutates to escape the immune system
The virus often mutates by simply deleting small pieces of its genetic code.

The novel coronavirus has developed a number of worrisome mutations, resulting in multiple new variants popping up around the world. Now, a new study sheds light on how the virus mutates so easily and why these mutations help it "escape" the body's immune response.
The study researchers found that SARS-CoV-2, the virus that causes COVID-19, often mutates by simply deleting small pieces of its genetic code. Although the virus has its own "proofreading" mechanism that fixes errors as the virus replicates, a deletion won't show up on the proofreader's radar.
"It's devilishly clever," study senior author Paul Duprex, director of the Center for Vaccine Research at the University of Pittsburgh, told Live Science. "You can't fix what's not there."
What's more, for SARS-CoV-2, these deletions frequently show up in similar spots on the genome, according to the study, published Feb. 3 in the journal Science. These are sites where people's antibodies would bind to and inactivate the virus. But because of these deletions, certain antibodies cannot recognize the virus.
Duprex likened the deletions to a string of beads where one bead is popped out. That might not seem like a big deal, but to an antibody, it's "completely different," he said. "These tiny little absences have a big, big effect."
Sneaky deletions
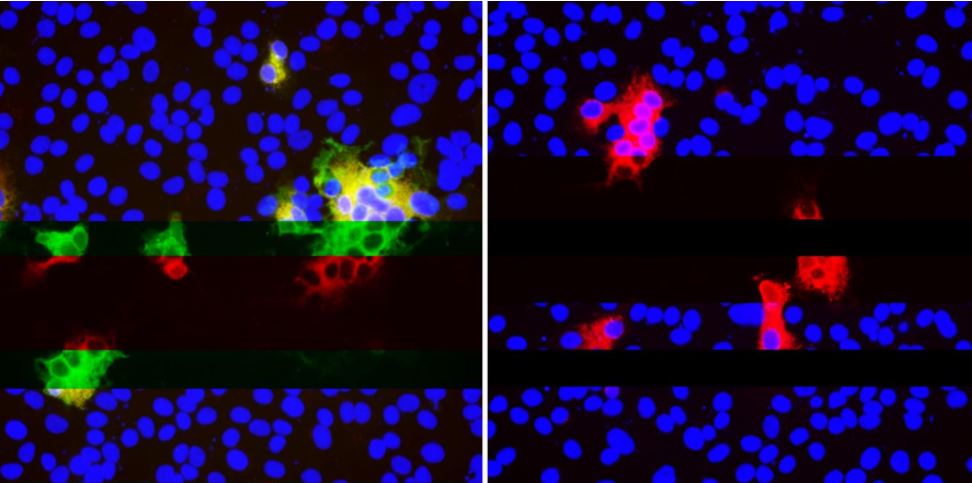
Duprex and his colleagues first noticed these deletions in a patient who was infected with the coronavirus for an unusually long time — 74 days. The patient had a weakened immune system, which prevented them from clearing the virus properly. During the lengthy infection, the coronavirus started to evolve as it played "cat and mouse" with the patient's immune system, ultimately developing deletions, the researchers said.
They wondered how common such deletions were. They used a database called GISAID to analyze some 150,000 genetic sequences of SARS-CoV-2 collected from samples around the world. And a pattern emerged. "These deletions started to line up to very distinct sites," said study lead author Kevin McCarthy, assistant professor of molecular biology and molecular genetics at the University of Pittsburgh.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
"We kept seeing them over and over and over again," in SARS-CoV-2 samples collected from different parts of the world at different times, he said. It seemed that these viruses strains were independently developing these deletions due to a "common selective pressure," the researchers wrote in their paper.
The researchers dubbed these sites "recurrent deletion regions." They noticed that these regions tended to occur in spots on the virus's spike protein where antibodies bind in order to disable the virus. "That gave us the first clue that possibly these deletions were leading to the 'escape' or the evolution [of the virus] away from the antibodies that are binding," McCarthy said.
Predicting new variants
The researchers started their project in the summer of 2020, when the coronavirus wasn't thought to be mutating in a significant way. But the deletions that popped up in their data said otherwise. In October 2020, they spotted a variant with these deletions that would later come to be known as the "U.K. variant," or B.1.1.7. This variant gained global attention beginning in December 2020, when it took off rapidly in the United Kingdom.
"Our survey for deletion variants captured the first representative of what would become the B.1.1.7 lineage," the authors wrote. Their finding underscores the importance of closely monitoring the virus's evolution by tracking these deletions and other mutations.
"We need to develop the tools, and we need to reinforce our vigilance for looking for these things and following them … so we can begin to predict what's going on," McCarthy said.
Although the virus may mutate to evade some antibodies, other antibodies can still effectively bind to and inactivate the virus.
"Going after the virus in multiple different ways is how we beat the shape-shifter," Duprex said in a statement. "Combinations of different antibodies [i.e. different monoclonal antibody treatments] … different types of vaccines. If there's a crisis, we'll want to have those backups."
The findings also show why it's important to wear a mask and implement other measures to prevent the virus from spreading — the more people it infects, the more chances it has to replicate and potentially mutate.
"Anything that we can do to dampen the number of times it replicates … will buy us a little bit of time," Duprex said.
Originally published on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.










