Omicron's not the last variant we'll see. Will the next one be bad?
Experts say it wouldn't be surprising if another concerning variant cropped up this year.

The new year rode in on a wave of omicron cases, but will this be the last of the variants, or will a brand-new "variant of concern" emerge in 2022?
Experts told Live Science that they wouldn't be surprised if a troublesome new coronavirus variant crops up this year — but that it's difficult to predict how quickly that variant would spread, how well it would evade the human immune system or whether it would cause more severe disease than prior versions of the virus.
The omicron variant gained an edge over delta both because it is highly transmissible and because it can evade the immune defenses of vaccinated and previously infected people. This has allowed the variant to infect part of the population that delta can't readily infect, Kartik Chandran, a virologist and professor of microbiology and immunology at the Albert Einstein College of Medicine in New York City, told Live Science. Similarly, to compete with omicron, future variants of concern would need to make similar gains in both transmissibility and immune evasiveness, Chandran said.
Related: Coronavirus variants: Facts about omicron, delta and other COVID-19 mutants
"There's no reason to believe that the virus has run out of room, genetically," he said. "I would expect that we're going to see more variants, and we're going to see similar types of wave-like behavior," meaning a surge in infection rates following a new variant's introduction.
But while the next problem variant may easily spread and outwit the immune system, the trajectory for its other traits, such as virulence — the severity of disease caused by the virus — remains unclear.
What could the next variant of concern be like?
Given the current rate of coronavirus infection worldwide, and the mutation rate of SARS-CoV-2, "it is predictable that new variants will emerge," Karen Mossman, a professor of pathology and molecular medicine at McMaster University in Ontario, told Live Science in an email. But as we've learned over the last two years of the pandemic, not every new variant will be competitive enough to take over, she said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Future variants could gain a competitive edge via several routes. In theory, one of these potential trajectories could result in a virus that's more transmissible than omicron while causing less severe disease, Mossman said.
"Viruses need to propagate and spread to new hosts. The most successful viruses do this by rapidly spreading without causing symptoms," because the infected host can easily move about and pass the bug to additional hosts, Mossman said. "It is not advantageous to a virus to kill off its host before it can spread."
Omicron may be less likely to cause severe disease than prior variants, Live Science previously reported. In part, that may be because it grows more easily in the upper airways and less well in the lungs — which may also help the variant spread more easily. In this case, it does seem like the virus may have evolved to be less virulent as a result of its increased ability to jump between hosts.
But there's no guarantee that the next variant of concern will make the same trade-off, Mossman noted. "A collection of mutations that provide a selective advantage may also induce more severe disease," she said.
For instance, mutations that grant the virus the ability to replicate incredibly quickly, or escape the clutches of the antibodies that prevent it from entering cells, could also make the bug more likely to trigger severe infection. Delta showed such a combination of traits, in that it spread more easily than all previous coronavirus variants while still doubling the risk of hospitalization for unvaccinated people, as compared with alpha, The New York Times reported. HIV and Ebola are examples of viral diseases that have not evolved to be less severe despite being around for decades; smallpox was another example, prior to its eradication.
Related: 20 of the worst epidemics and pandemics in history
The idea that the virus might become less virulent over time is "certainly not unreasonable as a hypothesis," Chandran said, but he agreed with Mossman that such an outcome isn't assured. Often, as viruses replicate and pick up mutations, the individual mutations within the genome interact with each other and can produce unexpected traits, he noted. This phenomenon, called epistasis, makes the evolution and behavior of future variants incredibly difficult to predict.

Big unknowns
In general, there are physical and genetic constraints that limit how much SARS-CoV-2 can evolve, Chandran noted. Some of these constraints prevent the virus from becoming infinitely more infectious, and for this reason, scientists expect that the transmissibility of the virus will eventually level off and stop increasing, Nature reported.
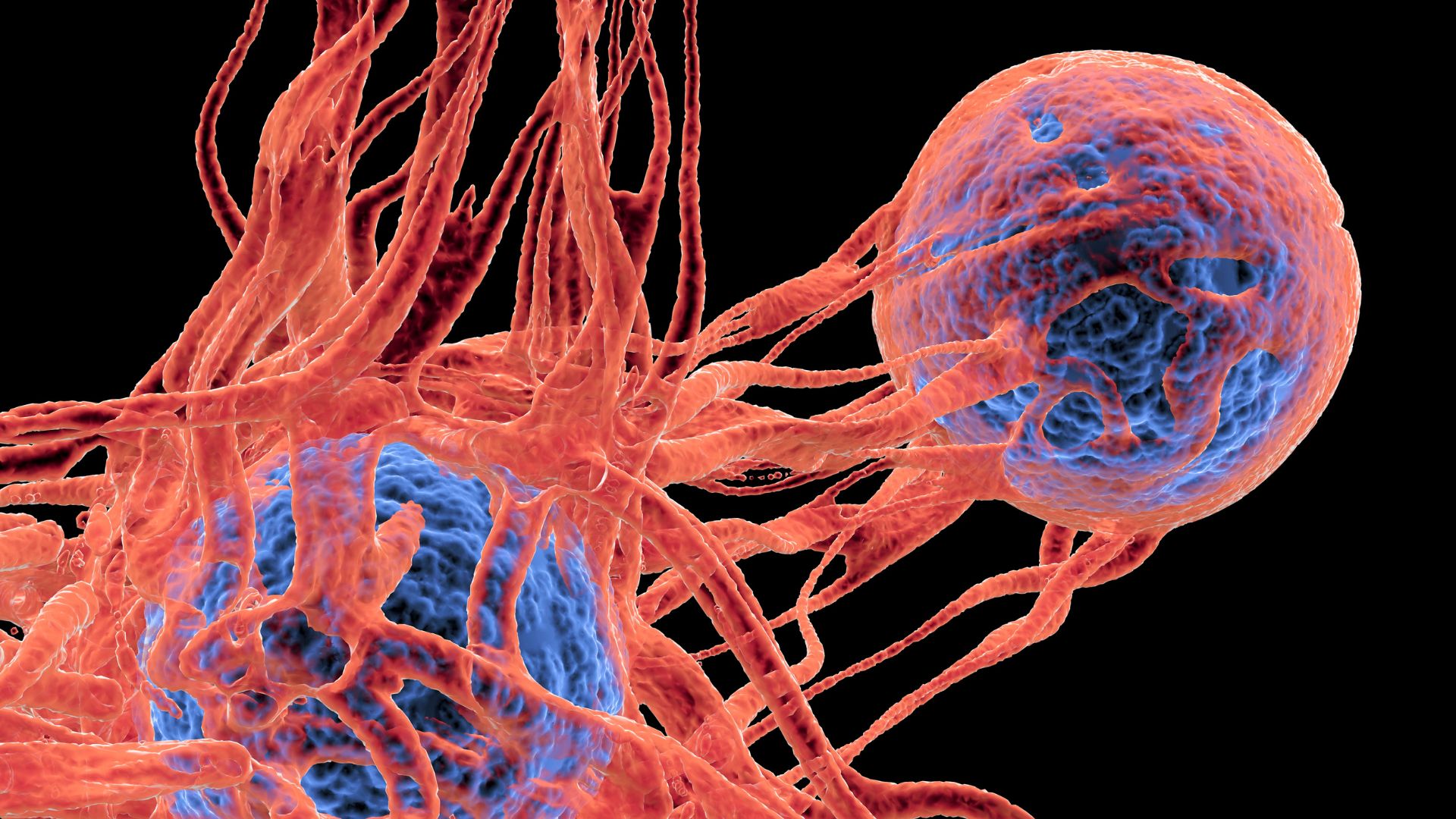
On a physical level, "viruses have to walk this fine line between stability and instability," and this balancing act limits their transmissibility, Chandran said. A virus is basically a microscopic box full of genetic material, and that box must be sturdy enough to keep the genetic material safe in the body and in the outside world. But to infect cells, the box must open to let the virus's genetic material out. Too stable, and the virus can't open up and infect cells as efficiently; too unstable, and the virus won't survive for long after being spewed out in someone's sneeze, Chandran said.
And on a genetic level, the virus can only accumulate so many mutations before it begins to malfunction, he said.
For example, the virus needs its spike protein to fit snugly into a receptor on human cells in order to trigger infection. Spike mutations can help the microbe hide from antibodies to past variants; omicron carries about 30 mutations in its spike, some of which help the variant evade the immune system. But there's likely a limit to how many mutations the spike can accommodate before its ability to plug into human cells starts to falter, Chandran said.
In this respect, the virus likely still has some genetic wiggle room. Based on a recent study, published Dec. 2 in the journal Science, SARS-CoV-2 can likely withstand a large number of escape mutations — those that help the bug dodge antibodies — while still retaining its ability to plug into human cells. "The great structural flexibility we saw in the SARS-CoV-2 spike protein suggests that omicron is not likely to be the end of the story for this virus," senior study author Dr. Jonathan Abraham, an assistant professor of microbiology at Harvard Medical School and an infectious disease specialist at Brigham and Women’s Hospital, told The Harvard Gazette.
Other unknowns make the future of SARS-CoV-2's evolution difficult to predict. One big question is where the next variant of concern will come from, since it may not descend from the omicron lineage, Chandran said. Omicron stemmed from a different branch of the coronavirus family tree than delta, even though delta was predominant at the time; the next variant may have a similar origin story.
Meanwhile, animal hosts for the coronavirus are yet another wildcard.
SARS-CoV-2 can infect a variety of animals, including mink, ferrets, cats, white-tailed deer and various primates, Nature reported. This has raised concerns that, while circulating in animals, the virus could pick up mutations that render the bug more infectious or lethal to humans, or else undermine the efficacy of our vaccines. For this scenario to unfold, the coronavirus would need to make the leap back to humans after infecting an animal, and in some cases, the virus might mutate so much that it can't hop back into people, Chandran noted. "The genetic trajectory of the virus could be quite different in these other hosts," he said.
That said, cases of animal-to-human transmission were reported on mink farms early in the pandemic, and it's possible that other species could also pass the virus back to people, Live Science previously reported. For this reason, scientists should continue to track SARS-CoV-2 spread in both humans and animals, as animal reservoirs of the virus could definitely be an issue in the future, Chandran said.
Reducing the risk of problem variants
Is there anything we can do to reduce the risk of new problem variants emerging?
"What we need to do is reduce … the space the virus has to replicate. And the way we're going to do that is by vaccinating people," Chandran said. As of Jan. 10, about 4.67 billion people worldwide have received at least one dose of a COVID-19 vaccine, which leaves nearly 40% of the world's population completely unvaccinated, according to The New York Times.
Even if vaccines offer only partial protection against a future variant, as they do with omicron, they would likely still reduce people's chances of catching and passing on the virus. However, vaccination would work best in combination with other measures, such as masking, physical distancing and frequent testing, Chandran said. But importantly, increasing the number of people vaccinated would also ease the strain on the health care system by preventing severe disease, he noted.
Early evidence, posted Jan. 3 to the preprint database medRxiv, suggests that even though the omicron variant can dodge some vaccine-induced antibodies, other immune defenses raised by the vaccine still block severe infections. The study, which has not been peer-reviewed, shows that the vaccines generate "durable responses" from helper T cells, which rev up the body's immune response upon sensing SARS-CoV-2, and killer T cells, which can kill infected cells. These T cells show cross-reactivity to both the delta and omicron variants, meaning they can recognize and target both versions of the virus for destruction, the study found. Similarly, these T cells could offer protection against potential future variants of concern.
Broadly speaking, "As more and more people become infected and/or vaccinated, particularly multiple times, they will build up higher levels of immunity, potentially against different variants," Mossman told Live Science. "As this general level of immunity increases within populations, and around the world, the overall evolution of SARS-CoV-2 will likely decline, and the pandemic will become endemic."
This is how the pandemic could end — but we'll likely have to face new variants of concern until then.
Originally published on Live Science.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.