Wuhan lab says there's no way coronavirus originated there. Here's the science.
An unprecedented amount of research has been focused solely on understanding the novel coronavirus that has taken nearly 150,000 lives across the globe. And while scientists have gotten to know some of the most intimate details of the virus called SARS-CoV-2, one question has evaded any definitive answers — Where did the virus come from?
Live Science contacted several experts, and the reality, they said, is that we may never know where this deadly coronavirus originated. Among the theories circulating: That SARS-CoV-2 arose naturally, after passing from bats to a secondary animal and then to humans; that it was deliberately engineered and then accidentally released by humans; or that researchers were studying a naturally-occurring virus that subsequently escaped from a high-security biolab, the Wuhan Institute of Virology (WIV) in China. The head of the lab at WIV, for her part, has emphatically denied any link to the institute.
Just today (April 18), the vice director of WIV Zhiming Yuan CGTN, the Chinese state broadcaster, said "there is no way this virus came from us," NBC News reported. "We have a strict regulatory regime and code of conduct of research, so we are confident."
Furthermore, the notion that SARS-CoV-2 was genetically engineered is pure conspiracy, experts told Live Science, but it's still impossible to rule out the notion that Chinese scientists were studying a naturally-occurring coronavirus that subsequently "escaped" from the lab. To prove any of these theories takes transparent data and information, which is reportedly not happening in China, scientists say. Several experts have said to Live Science and other media outlets have reported that the likeliest scenario is that SARS-CoV-2 is naturally occurring.
Related: 13 coronavirus myths busted by science
"Based on no data, but simply [a] likely scenario is that the virus went from bats to some mammalian species, currently unknown despite speculation, [and] spilled over to humans," said Gerald Keusch, associate director of the Boston University National Emerging Infectious Diseases Laboratories. This spillover event may have happened before the virus found its way into a live animal market, "which then acted as an amplifying setting with many more infections that subsequently spread and the rest is history," Keusch said. "The timeline is fuzzy and I don't think we have real data to say when these things began, in large part because the data are being held back from inspection," Keusch told Live Science.
Murky origins
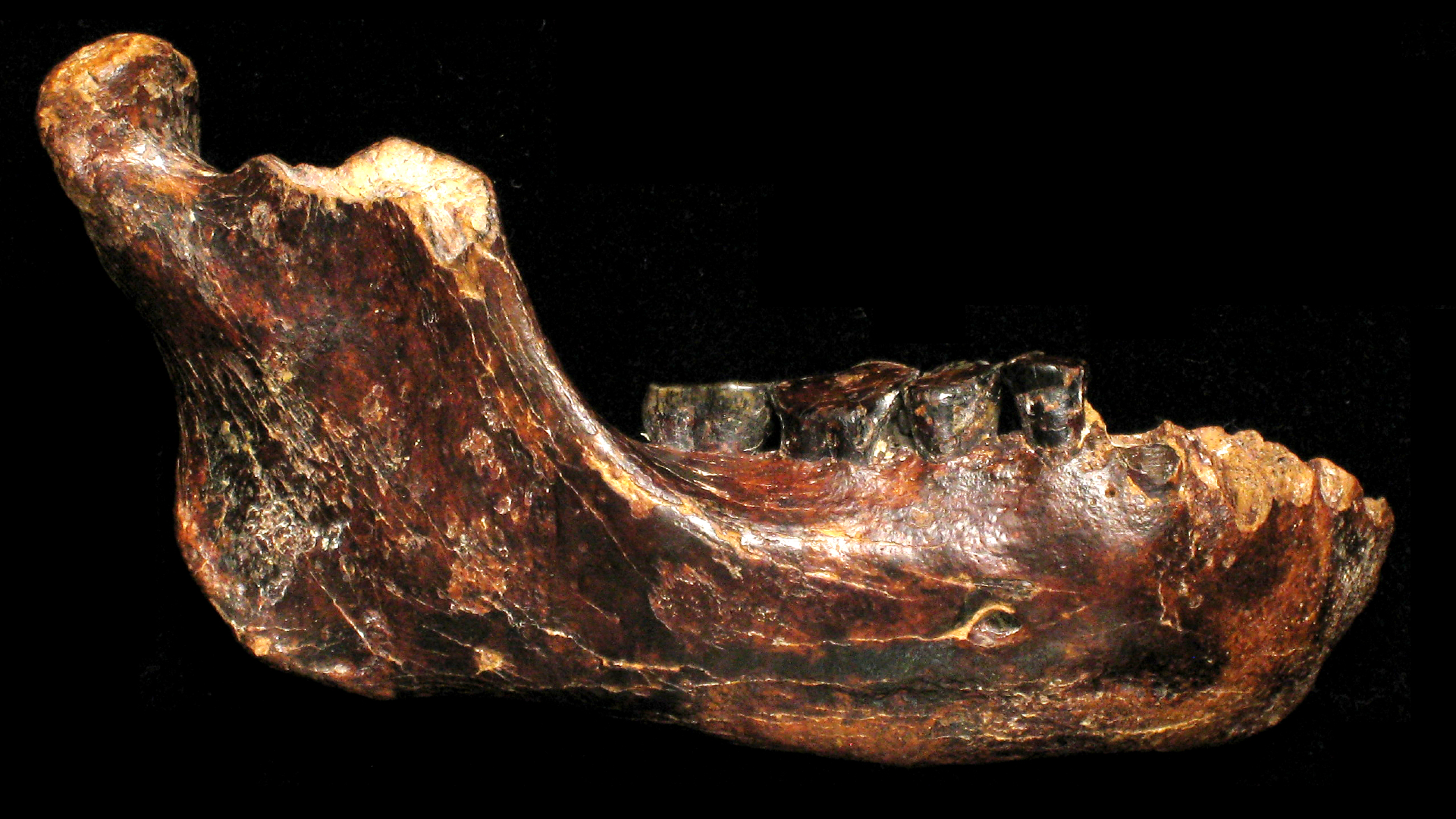
The SARS-CoV-2 virus is most closely related to coronaviruses found in certain populations of horseshoe bats that live about 1,000 miles (1,600 kilometers) away in Yunnan province, China. The first known outbreak of SARS-CoV-2 in humans occurred in Wuhan and initially was traced to a wet seafood market (which sold live fish and other animals), though some of the earliest cases have no link to that market, according to research published Feb. 15 in the journal The Lancet.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Related: 11 (sometimes) deadly diseases that hopped across species
What's more, despite several proposed candidates, from snakes to pangolins to dogs, researchers have failed to find a clear "intermediate host" — an animal that would have served as a springboard for SARS-CoV-2 to jump from bats to humans. And if horseshoe bats were the primary host, how did the bat virus hop from its natural reservoir in a subtropical region to the bustling city of Wuhan hundreds of miles away?
The lab at the center of pandemic controversy

These questions have led some people to look elsewhere in the hunt for the virus's origin, and some have focused on the Wuhan Institute of Virology (WIV).
In 2015, WIV became China's first lab to reach the highest level of bioresearch safety, or BSL-4, meaning the lab could host research on the world's most dangerous pathogens, such as Ebola and Marburg viruses. (SARS-CoV-2 would require a BSL-3 or higher, according to the Centers for Disease Control and Prevention.) Labs like these must follow strict safety guidelines that include filtering air, treating water and waste before they exit, and requiring lab personnel to shower and change their clothes before and after entering the facility, Nature News reported in 2017.
These types of labs do spur concerns among some scientists who worry about the risks involved and the potential impact on public health if anything were to go wrong, Nature News reported.
Related: The 12 deadliest viruses on Earth
WIV was not immune to those concerns. In 2018, after scientist diplomats from the U.S. embassy in Beijing visited the WIV, they were so concerned by the lack of safety and management at the lab that the diplomats sent two official warnings back to the U.S. One of the official cables, obtained by The Washington Post, suggested that the lab's work on bat coronaviruses with the potential for human transmission could risk causing a new SARS-like pandemic, Post columnist Josh Rogin wrote.
"During interactions with scientists at the WIV laboratory, they noted the new lab has a serious shortage of appropriately trained technicians and investigators needed to safely operate this high-containment laboratory," the officials said in their cable dated to Jan. 19, 2018.
When reports of the coronavirus first popped up in China, the U.S. Deputy National Security Advisor Matthew Pottinger reportedly suspected a potential link to China labs. In mid-January, according to a New York Times report, Pottinger asked intelligence agencies like the C.I.A., particularly individuals with expertise on Asia and weapons of mass destruction, to investigate this idea. They came up empty-handed, the Times reported.
Studying dangerous pathogens
Meanwhile, the lab at the center of these speculations had long been sounding the alarm about the risk of the SARS-like coronaviruses they studied to spawn a pandemic.
The head of the lab's bat-coronavirus research, Shi Zhengli, published research on Nov. 30, 2017 in the journal PLOS Pathogens that traced the SARS coronavirus pandemic in 2003 to a single population of horseshoe bats in a remote cave in Yunnan province. The researchers also noted that other SARS-like coronaviruses discovered in that cave used the ACE2 receptor to infect cells and could "replicate efficiently in primary human airway cells," they wrote. (Both SARS and SARS-CoV-2 use the ACE2 receptor as the entry point into cells.)
Zhengli and her colleagues stressed the importance of monitoring and studying the SARS coronaviruses to help prevent another pandemic.
"Thus, we propose that monitoring of SARS-CoV evolution at this and other sites should continue, as well as examination of human behavioral risk for infection and serological surveys of people, to determine if spillover is already occurring at these sites and to design intervention strategies to avoid future disease emergence," they wrote.
Related: 20 of the worst epidemics and pandemics in history
The WIV lab, along with researchers in the U.S. and Switzerland, showed in 2015 the scary-good capability of bat coronaviruses to thrive in human cells. In that paper, which was published in 2015 in the journal Nature Medicine, they described how they had created a chimeric SARS-like virus out of the surface spike protein of a coronavirus found in horseshoe bats, called SHC014, and the backbone of a SARS virus that could be grown in mice. The idea was to look at the potential of coronaviruses circulating in bat populations to infect humans. In a lab dish, the chimeric coronavirus could infect and replicate in primary human airway cells; the virus also was able to infect lung cells in mice.
That study was met with some pushback from researchers who considered the risk of that kind of research to outweigh the benefits. Simon Wain-Hobson, a virologist at the Pasteur Institute in Paris, was one of those scientists. Wain-Hobson emphasized the fact that this chimeric virus "grows remarkably well" in human cells, adding that "If the virus escaped, nobody could predict the trajectory," Nature News reported.
Finding 'patient zero'
None of this can show the provenance of SARS-CoV-2.
But scientists can start to rule out an idea that the pandemic-causing coronavirus was engineered in that lab or further created as a bioweapon. Researchers say the overwhelming evidence indicates this is a natural-borne virus that emerged from an animal host, likely a bat, and was not engineered by humans.
Related: 28 devastating infectious diseases
"This origin story is not currently supported at all by the available data," said Adam Lauring, an associate professor of microbiology, immunology and infectious diseases at the University of Michigan Medical School. Lauring pointed to a study published March 17 in the journal Nature Medicine, which provided evidence against the idea that the virus was engineered in a lab.
In that Nature medicine study — one of the strongest rebukes of this idea — Kristian Andersen, an associate professor of immunology and microbiology at Scripps Research, and his colleagues analyzed the genome sequences of SARS-CoV-2 and coronaviruses in animals. They found that a key part of SARS-CoV-2, the spike protein that the virus uses to attach to ACE2 receptors on the outsides of human cells, would almost certainly have emerged in nature and not as a lab creation.
"This analysis of coronavirus genome sequences from patients and from various animals suggests that the virus likely arose in an animal host and then may have undergone further changes once it transmitted and circulated in people," Lauring told Live Science.
That may rule out deliberate genetic engineering, but what about other scenarios that point to bats as the natural hosts, but WIV as the source of the outbreak?
Although researchers will likely continue to sample and sequence coronaviruses in bats to determine the origin of SARS-CoV-2, "you can't answer this question through genomics alone," said Dr. Alex Greninger, an assistant professor in the Department of Laboratory Medicine and an assistant director of the Clinical Virology Laboratory at the University of Washington Medical Center. That's because it's impossible to definitively tell whether SARS-CoV-2 emerged from a lab or from nature based on genetics alone. For this reason, it's really important to know which coronaviruses were being studied at WIV. "It really comes down to what was in the lab," Greninger told Live Science.
However, Lauring said that based on the Nature Medicine paper, "the SARS-CoV-2 virus has some key differences in specific genes relative to previously identified coronaviruses — the ones a laboratory would be working with. This constellation of changes makes it unlikely that it is the result of a laboratory 'escape,'" he said.
As for what viruses were being studied at WIV, Zhengli says she did a thorough investigation. When she first was alerted to the viral outbreak in Wuhan on the night of Dec. 30, 2019, Zhengli immediately put her lab to work sequencing the genomes of SARS-CoV-2 from infected patients and comparing the results with records of coronavirus experiments in her lab. She also looked for any mishandling of viral material used in any experiments, Scientific American reported. She didn't find any match between the viruses her team was working with from bat caves and those found in infected patients. "That really took a load off my mind," she told Scientific American. "I had not slept a wink for days."
At the beginning of February, Zhengli sent a note over WeChat to reassure her friends that there was no link, saying "I swear with my life, [the virus] has nothing to do with the lab," the South China Morning Post reported Feb. 6. Zhengli and another colleague, Peng Zhou, did not reply to a Live Science email requesting comment.
The Wuhan lab does work with the closest known relative of SARS-CoV-2, which is a bat coronavirus called RaTG13, evolutionary virologist Edward Holmes, of the Charles Perkins Center and the Marie Bashir Institute for Infectious Diseases and Biosecurity at the University of Sydney, said in a statement from the Australian Media Center. But, he added, "the level of genome sequence divergence between SARS-CoV-2 and RaTG13 is equivalent to an average of 50 years (and at least 20 years) of evolutionary change." (That means that in the wild, it would take about 50 years for these viruses to evolve to be as different as they are.)
Though no scientists have come forth with even a speck of evidence that humans knowingly manipulated a virus using some sort of genetic engineering, a researcher at Flinders University in South Australia lays out another scenario that involves human intervention. Bat coronaviruses can be cultured in lab dishes with cells that have the human ACE2 receptor; over time, the virus will gain adaptations that let it efficiently bind to those receptors. Along the way, that virus would pick up random genetic mutations that pop up but don't do anything noticeable, said Nikolai Petrovsky, in the College of Medicine and Public Health at Flinders.
"The result of these experiments is a virus that is highly virulent in humans but is sufficiently different that it no longer resembles the original bat virus," Petrovsky said in a statement from the Australian Media Center. "Because the mutations are acquired randomly by selection, there is no signature of a human gene jockey, but this is clearly a virus still created by human intervention."
If that virus infected a staff member and that person then traveled to the nearby seafood market, the virus could have spread from there, he said. Or, he added, an "inappropriate disposal of waste from the facility" could have infected humans directly or from a susceptible intermediary, such as a stray cat.
Though we may never get a definitive answer, at least in the near-term, some say it doesn't matter.
"No matter the origin, evolution in nature and spillover to humans, accidental release from a lab, or deliberate release or genetic manipulation of a pathogen in the lab the way you develop countermeasures is the same," Keusch told Live Science. "Since one can never say 100% for anything, I think we always need to be aware of all possibilities in order to contravene. But the response to develop what is needed to respond, control and eliminate the outbreak remains the same."
Live Science senior writer Rachael Rettner contributed to this report.
Originally published on Live Science.
- The 9 Deadliest Viruses on Earth
- 28 Devastating Infectious Diseases
- 11 Surprising Facts About the Respiratory System
OFFER: Save 45% on 'How It Works' 'All About Space' and 'All About History'!
For a limited time, you can take out a digital subscription to any of our best-selling science magazines for just $2.38 per month, or 45% off the standard price for the first three months.
Jeanna Bryner is managing editor of Scientific American. Previously she was editor in chief of Live Science and, prior to that, an editor at Scholastic's Science World magazine. Bryner has an English degree from Salisbury University, a master's degree in biogeochemistry and environmental sciences from the University of Maryland and a graduate science journalism degree from New York University. She has worked as a biologist in Florida, where she monitored wetlands and did field surveys for endangered species, including the gorgeous Florida Scrub Jay. She also received an ocean sciences journalism fellowship from the Woods Hole Oceanographic Institution. She is a firm believer that science is for everyone and that just about everything can be viewed through the lens of science.