Your risk of severe COVID-19 may be affected by blood type, new genetic analysis suggests
People with blood type O may have a reduced risk of developing severe symptoms

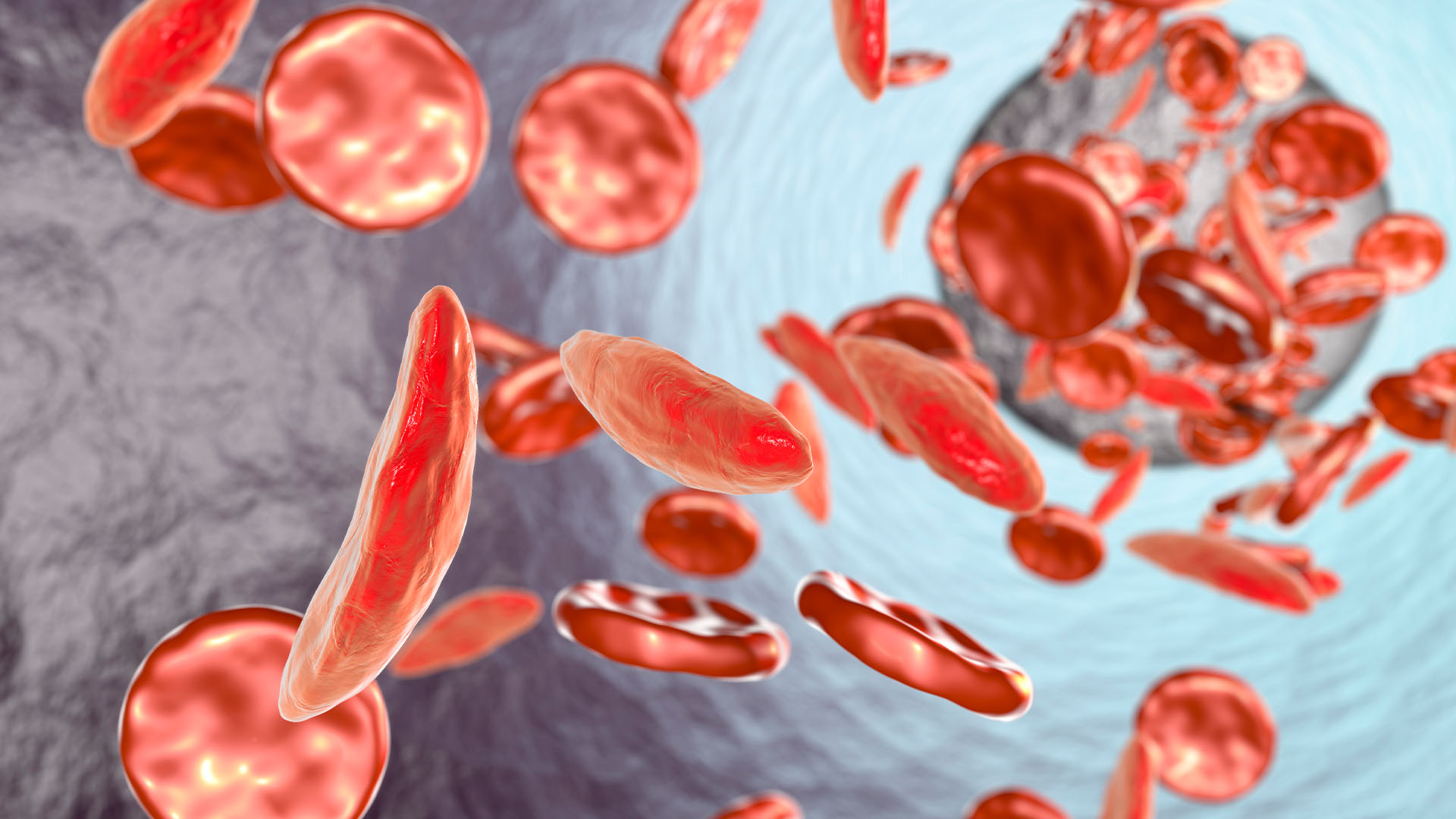
Genes associated with certain blood types may increase the risk of severe COVID-19 infections, leading to respiratory failure and death, a new study suggests.
The study authors found that people with blood type A were 50% more likely than people with other blood types to experience severe COVID-19 symptoms and respiratory failure. By comparison, people with blood type O had a 50% reduced risk of developing severe symptoms of COVID-19 — the disease caused by the novel coronavirus — or those severe enough to require oxygen or a ventilator.
Scientists uncovered the connection between blood type and COVID-19 outcome using a genome-wide association study. By looking at the single-letter changes in many genes across a large population, researchers can pinpoint gene variants that may be tied to disease risk, according to the National Human Genome Research Institute.
Related: Coronavirus outbreak: Live updates
Two prior studies have hinted at the possibility of a link between blood types and risk factors for COVID-19, Live Science previously reported. Different teams of researchers found that people with blood type A had a higher risk of developing COVID-19, compared with people who had other blood types, and that people with blood type O were less likely to contract the disease.
However, these studies were released on the preprint database medRxiv — on March 27 and on April 11 — and were not peer-reviewed.
In the new study, researchers identified two regions in the genome where genetic variants were linked to severe cases of COVID-19 and a higher risk of death; in one of these regions was a gene that determines blood type. They published their findings online June 17 in the New England Journal of Medicine.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The researchers sampled the genomes of 1,610 COVID-19 patients and more than 1,300 healthy blood donors from Italy and Spain, and analyzed more than 8 million single-letter changes in the DNA code, called single nucleotide polymorphisms, or SNPs (pronounce "snips"). There are millions of SNPs sprinkled throughout a person's genome, and they can be used as markers for locating genes associated with disease, according to the U.S. National Library of Medicine.
The study authors pinpointed regions of the genome that were linked to respiratory failure from COVID-19 — symptoms severe enough to require supplemental oxygen or the use of a mechanical ventilator. One signal originated in a region that included genes linked to immune response in the lungs. The other signal came from a region that also codes for blood type, enabling the researchers to confirm "a potential involvement of the ABO blood-group system in COVID-19," they wrote in the study. This link suggests that blood type may be connected to the severity of respiratory symptoms.
The other region they identified contained six genes, some of which interact with the ACE2 receptor that SARs-CoV-2 targets, while others are tied to chemicals that interact with immune cells in the lung. It's not clear which of these genes play a role in disease susceptibility.
"A genetic test and a person’s blood type might provide useful tools for identifying those who may be at greater risk of serious illness," Francis Collins, director of the National Institutes of Health, said in a statement about the new study.
"The hope is that these and other findings yet to come will point the way to a more thorough understanding of the biology of COVID-19," Collins said.
However, many other factors also determine how dramatically an individual is affected by the illness.
Underlying health conditions such as heart disease, chronic lung disease and diabetes greatly increase the chances of getting very sick or dying from COVID-19. Indeed, while older people are generally considered to be more vulnerable to severe cases of COVID-19, that could be explained by the chronic medical conditions that often accompany aging, Live Science previously reported.
- Coronavirus in the US: Latest COVID-19 news and case counts
- 20 of the worst epidemics and pandemics in history
- The 12 deadliest viruses on Earth
Originally published on Live Science.
OFFER: Save 45% on 'How It Works' 'All About Space' and 'All About History'!
For a limited time, you can take out a digital subscription to any of our best-selling science magazines for just $2.38 per month, or 45% off the standard price for the first three months.

Mindy Weisberger is an editor at Scholastic and a former Live Science channel editor and senior writer. She has reported on general science, covering climate change, paleontology, biology and space. Mindy studied film at Columbia University; prior to Live Science she produced, wrote and directed media for the American Museum of Natural History in New York City. Her videos about dinosaurs, astrophysics, biodiversity and evolution appear in museums and science centers worldwide, earning awards such as the CINE Golden Eagle and the Communicator Award of Excellence. Her writing has also appeared in Scientific American, The Washington Post and How It Works Magazine. Her book "Rise of the Zombie Bugs: The Surprising Science of Parasitic Mind Control" will be published in spring 2025 by Johns Hopkins University Press.