COVID-19 treatment might already exist
Here's how researchers might find these coronavirus drugs.
Why don't we have drugs to treat COVID-19 and how long will it take to develop them?
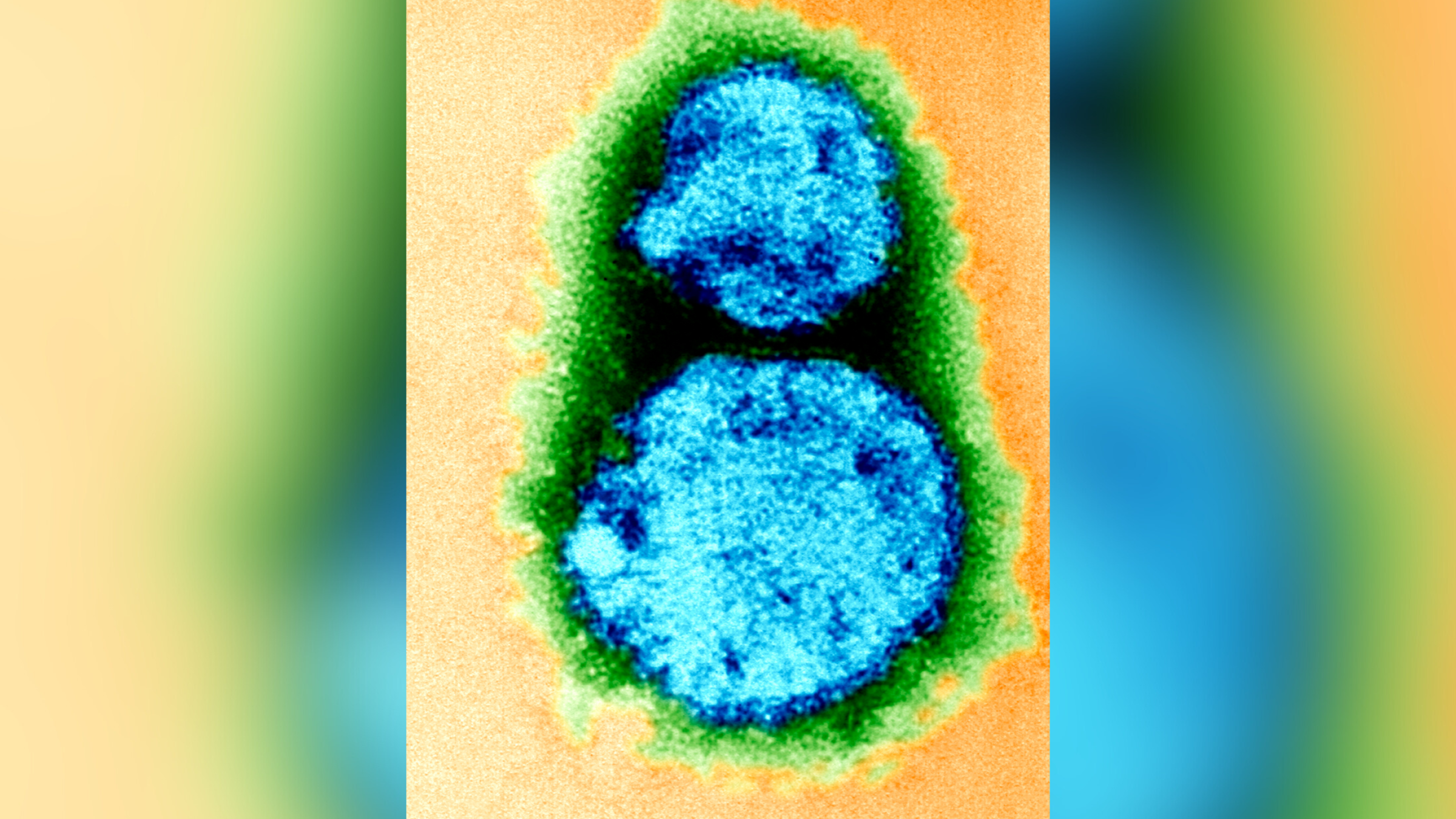
SARS-CoV-2 — the coronavirus that causes the disease COVID-19 — is completely new and attacks cells in a novel way. Every virus is different and so are the drugs used to treat them. That's why there wasn't a drug ready to tackle the new coronavirus that only emerged a few months ago.
As a systems biologist who studies how cells are affected by viruses during infections, I'm especially interested in the second question. Finding points of vulnerability and developing a drug to treat a disease typically takes years. But the new coronavirus isn't giving the world that kind of time. With most of the world on lockdown and the looming threat of millions of deaths, researchers need to find an effective drug much faster.
This situation has presented my colleagues and I with the challenge and opportunity of a lifetime: to help solve this huge public health and economic crisis posed by the global pandemic of SARS-CoV-2.
Facing this crisis, we assembled a team here at the Quantitative Biosciences Institute (QBI) at the University of California, San Francisco, to discover how the virus attacks cells. But instead of trying to create a new drug based on this information, we are first looking to see if there are any drugs available today that can disrupt these pathways and fight the coronavirus.
The team of 22 labs, that we named the QCRG, is working at breakneck speed — literally around the clock and in shifts — seven days a week. I imagine this is what it felt like to be in wartime efforts like the Enigma code-breaking group during World War II, and our team is similarly hoping to disarm our enemy by understanding its inner workings.
A stealthy opponent
Compared with human cells, viruses are small and can't reproduce on their own. The coronavirus has about 30 proteins, whereas a human cell has more than 20,000.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
To get around this limited set of tools, the virus cleverly turns the human body against itself. The pathways into a human cell are normally locked to outside invaders, but the coronavirus uses its own proteins like keys to open these "locks" and enter a person's cells.
Once inside, the virus binds to proteins the cell normally uses for its own functions, essentially hijacking the cell and turning it into a coronavirus factory. As the resources and mechanics of infected cells get retooled to produce thousands and thousands of viruses, the cells start dying.
Lung cells are particularly vulnerable to this because they express high amounts of the "lock" protein SARS-CoV-2 uses for entry. A large number of a person's lung cells dying causes the respiratory symptoms associated with COVID-19.
There are two ways to fight back. First, drugs could attack the virus's own proteins, preventing them from doing jobs like entering the cell or copying their genetic material once they are inside. This is how remdesivir — a drug currently in clinical trials for COVID-19 — works.
A problem with this approach is that viruses mutate and change over time. In the future, the coronavirus could evolve in ways that render a drug like remdesivir useless. This arms race between drugs and viruses is why you need a new flu shot every year.
Alternatively, a drug can work by blocking a viral protein from interacting with a human protein it needs. This approach — essentially protecting the host machinery — has a big advantage over disabling the virus itself, because the human cell doesn't change as fast. Once you find a good drug, it should keep working. This is the approach that our team is taking. And it may also work against other emergent viruses.
Learning the enemy's plans
The first thing our group needed to do was identify every part of the cellular factory that the coronavirus relies on to reproduce. We needed to find out what proteins the virus was hijacking.
To do this, a team in my lab went on a molecular fishing expedition inside human cells. Instead of a worm on a hook, they used viral proteins with tiny chemical tags attached to them - termed a "bait." We put these baits into lab-grown human cells and then pulled them out to see what we caught. Anything that stuck was a human protein that the virus hijacks during infection.
By March 2, we had a partial list of the human proteins that the coronavirus needs to thrive. These were the first clues we could use. A team member sent a message to our group, "First iteration, just 3 baits … next 5 baits coming." The fight was on.
Once we had this list of molecular targets the virus needs to survive, members of the team raced to identify known compounds that might bind to these targets and prevent the virus from using them to replicate. If a compound can prevent the virus from copying itself in a person's body, the infection stops. But you can't simply interfere with cellular processes at will without potentially causing harm to the body. Our team needed to be sure the compounds we identified would be safe and nontoxic for people.
The traditional way to do this would involve years of pre-clinical studies and clinical trials costing millions of dollars. But there is a fast and basically free way around this: looking to the 20,000 FDA-approved drugs that have already been safety-tested. Maybe there is a drug in this large list that can fight the coronavirus.
Our chemists used a massive database to match the approved drugs and proteins they interact with to the proteins on our list. They found 10 candidate drugs last week. For example, one of the hits was a cancer drug called JQ1. While we cannot predict how this drug might affect the virus, it has a good chance of doing something. Through testing, we will know if that something helps patients.
Facing the threat of global border shutdowns, we immediately shipped boxes of these 10 drugs to two of the few labs in the world working with live coronavirus samples: at the Pasteur Institute in Paris and Mount Sinai in New York. By March 13, the drugs were being tested in cells to see if they prevent the virus from reproducing.
Dispatches from the battlefield
Our team will soon learn from our collaborators at Mt. Sinai and the Pasteur Institute whether any of these first 10 drugs work against SARS-CoV-2 infections. Meanwhile, the team has continued fishing with viral baits, finding hundreds of additional human proteins that the coronavirus co-opts. We will be publishing the results in the online repository BioRxiv soon.
The good news is that so far, our team has found 50 existing drugs that bind the human proteins we've identified. This large number makes me hopeful that we'll be able to find a drug to treat COVID-19. If we find an approved drug that even slows down the virus's progression, doctors should be able to start getting it to patients quickly and save lives.
[You need to understand the coronavirus pandemic, and we can help. Read our newsletter.]
This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.

Nevan Krogan was born in Saskatchewan, Canada, and obtained his undergraduate degree from the University of Regina and his Ph.D. in Medical Genetics from the University of Toronto, Canada. He is a professor of Cellular and Molecular Pharmacology at the University of San Francisco, where his lab focuses on unbiased proteomic and genomic studies of cellular interactions involved in infectious disease, neuropsychiatric disorders and cancer. He is also a senior investigator at the J. David Gladstone Institutes, director of the California Institute for Quantitative Biosciences and director of the Quantitative Biosciences Institute, as well as the director of the Thermo Fisher Scientific Proteomics Facility for Disease Target Discovery.