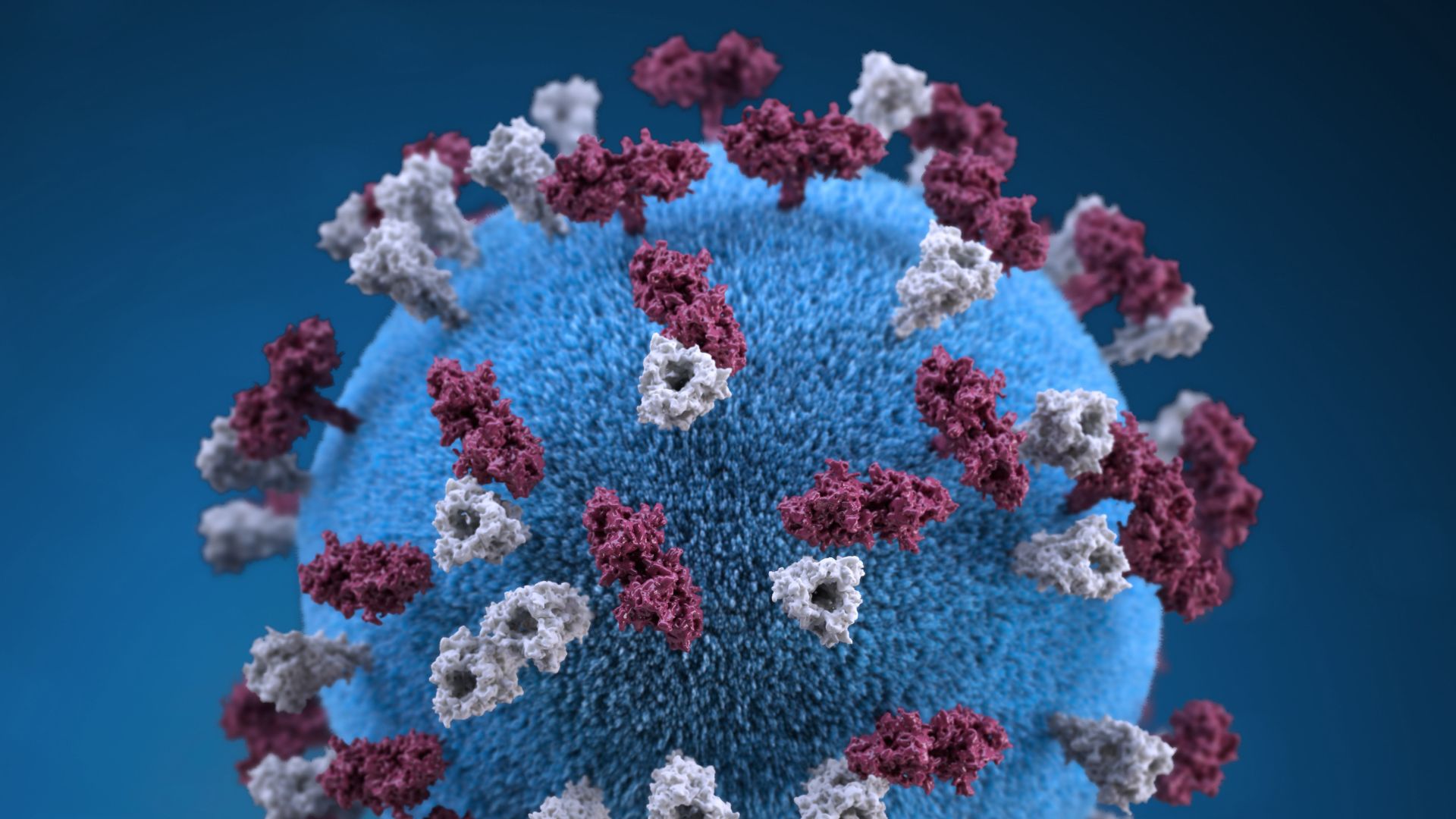
Coronavirus news of the week (VIDEO)
Since the discovery of the virus that causes COVID-19, the daily news cycle has become swamped with updates about how the pathogen spreads, what the bug does to the body and what solutions might finally bring an end to the pandemic.
But staying up-to-date on all the latest coronavirus news can be a challenge. To help keep you informed, we at Live Science have compiled a short list of standout news stories from the week — these are the ones that really caught our attention.
Related: 20 of the worst epidemics and pandemics in history
Confirmed reinfections

Researchers reported the first confirmed case of COVID-19 reinfection in a man in Hong Kong. The news initially came out on Aug. 24 in a press release from the University of Hong Kong, and the formal study was published Aug. 25 in the journal Clinical Infectious Diseases. But don't panic — an expert called the case "a textbook example of how immunity should work."
The 33-year-old was first diagnosed with COVID-19 on March 26 and had mild symptoms at the time, including a cough and fever. The man was released from the hospital on April 14 after testing negative for the virus twice, but he tested positive again during an airport screening on Aug. 15. The virus that infected the man the second time around carried several genetic differences to the first one, suggesting that the man had been infected by a new variant of the virus that subtly mutated through time, as all viruses do. But the man showed no symptoms of illness the second time, hinting that his body retained some immunity against the pathogen.
"While this is a good example of how primary infection can prevent disease from subsequent infection, more studies are needed to understand the range of outcomes from reinfection," Akiko Iwasaki, a professor of immunobiology and molecular, cellular and developmental biology at the Yale School of Medicine, wrote on Twitter.
Since this news came out, two more cases of reinfection have been confirmed in Europe, and one in the U.S., The New York Times reported. Like the Hong Kong case, the two European cases showed milder or no symptoms during the second infection; however, the U.S. patient developed severe symptoms and scientists are investigating several theories as to why. We don't yet know how commonly reinfection occurs, how often people develop severe symptoms the second time around or what these trends mean for vaccine development — that information will only come from further research.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
CDC changes its testing guidelines

The Centers for Disease Control and Prevention (CDC) abruptly changed its COVID-19 testing guidance, stating that those who have come in contact with an infected person don't necessarily need a test if they are not in a high-risk group or showing symptoms of the disease.
Prior to the change, the CDC recommended that all close contacts of people who have tested positive for COVID-19 also be tested, given that we know the virus can spread before people show symptoms, and that testing close contacts helps keep outbreaks in check. The Assistant Secretary for Health at the U.S. Department of Health and Human Services (HHS) Dr. Brett Giroir told CNN that the new guidelines are intended to encourage tests to be used "appropriately," and not to reduce the number of tests given overall. But public health officials say the guidance directly conflicts with scientific evidence.
"These testing recommendations make no scientific sense, unless there are plans to demand isolation of all known contacts of COVID-19," said Krys Johnson, an assistant professor of instruction in the Department of Epidemiology and Biostatistics at Temple University in Pennsylvania. Especially as schools and universities reopen, the U.S. should be testing more asymptomatic people for the virus, not fewer, she said.
In response to outcry from public health officials, CDC Director Dr. Robert Redfield clarified the new guidance on Aug. 27, saying "testing may be considered for all close contacts of confirmed or probable COVID-19 patients," but should be prioritized for symptomatic people, people with risk factors for severe infection and people at high risk of exposure. However, at the time of this verbal statement, the official guidance on the CDC website remained unchanged.
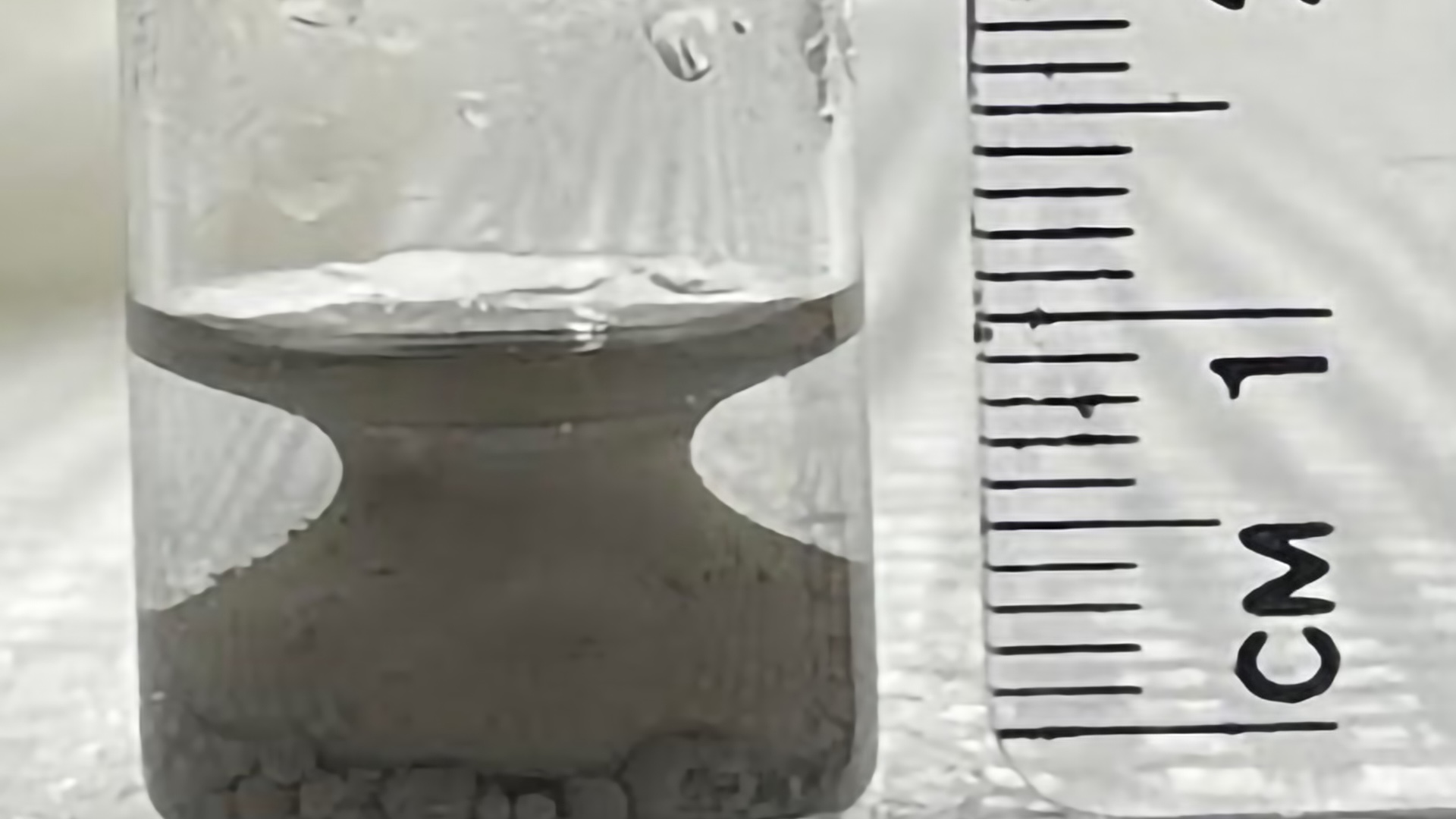
Authorization for plasma

Last week, we highlighted news that the U.S. Food and Drug Administration (FDA) would not authorize the use of blood plasma to treat COVID-19 patients without more data from clinical trials. This week, the FDA issued an emergency use authorization for the treatment without any additional data in hand.
Emergency use authorization allows doctors to administer an unapproved medical treatment "when there are no adequate, approved and available alternatives," and patients don't need to be enrolled in a clinical trial to receive the therapy, according to the FDA website. But infectious disease experts and public health officials argue that convalescent plasma therapy — which uses antibody-rich plasma from people who have recovered from a disease — has not earned this seal of approval.
To demonstrate that plasma helps COVID-19 patients recover, scientists must conduct randomized controlled trials (RCTs), wherein participants randomly receive either plasma or the standard of care; outcomes can then be compared between the two groups without bias. RCTs of plasma have proven difficult to organize, given that the supply of eligible plasma and number of people sick with COVID-19 varies from region to region.
With many RCTs for plasma still underway, the authorization of the treatment could make recruiting patients for these trials even more difficult. While patients in an RCT randomly receive either plasma or the standard of care, patients treated under the emergency authorization would not be subject to this randomization; the guarantee of plasma outside of an RCT could make participating in the trials a hard sell.
If RCTs do get derailed, it will be harder to collect solid evidence that plasma therapy works.
Originally published on Live Science.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.