Coronavirus news of the week (VIDEO)
Since the discovery of the virus that causes COVID-19, the daily news cycle has been flooded with updates about how the pathogen spreads, what the bug does to the body and what solutions might finally bring an end to the pandemic.
But staying up-to-date on all the latest coronavirus news can be a challenge. To help keep you informed, we at Live Science have compiled a short list of standout news stories from the week — these are the ones that really caught our attention.
Related: 20 of the worst epidemics and pandemics in history
Pause in vaccine trial

AstraZeneca and Oxford University have paused their trial of a COVID-19 vaccine after a participant developed a suspected adverse reaction.
This kind of hold is a "routine action" taken during clinical trials; whenever a trial participant develops an unexplained illness, the company stops administering the vaccine while an independent committee determines whether the reaction is related to the vaccine. In large clinical trials that include tens of thousands of people, participants can fall ill by chance, so each case of illness must be carefully reviewed to determine whether the vaccine triggered the reaction.
Related: Here are the most promising coronavirus vaccine candidates out there
In this instance, the participant developed neurological symptoms often associated with transverse myelitis, a condition where the spinal cord becomes inflamed. The participant is now recovering in the hospital and should be discharged soon, but her diagnosis still needs to be confirmed, AstraZeneca CEO Pascal Soriot told investors during a private call on Sep. 9, according to Stat News.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The AstraZeneca trials were paused once before when a different participant developed neurological symptoms. However, that first patient was later diagnosed with multiple sclerosis and the committee determined that the illness was not related to the vaccination.
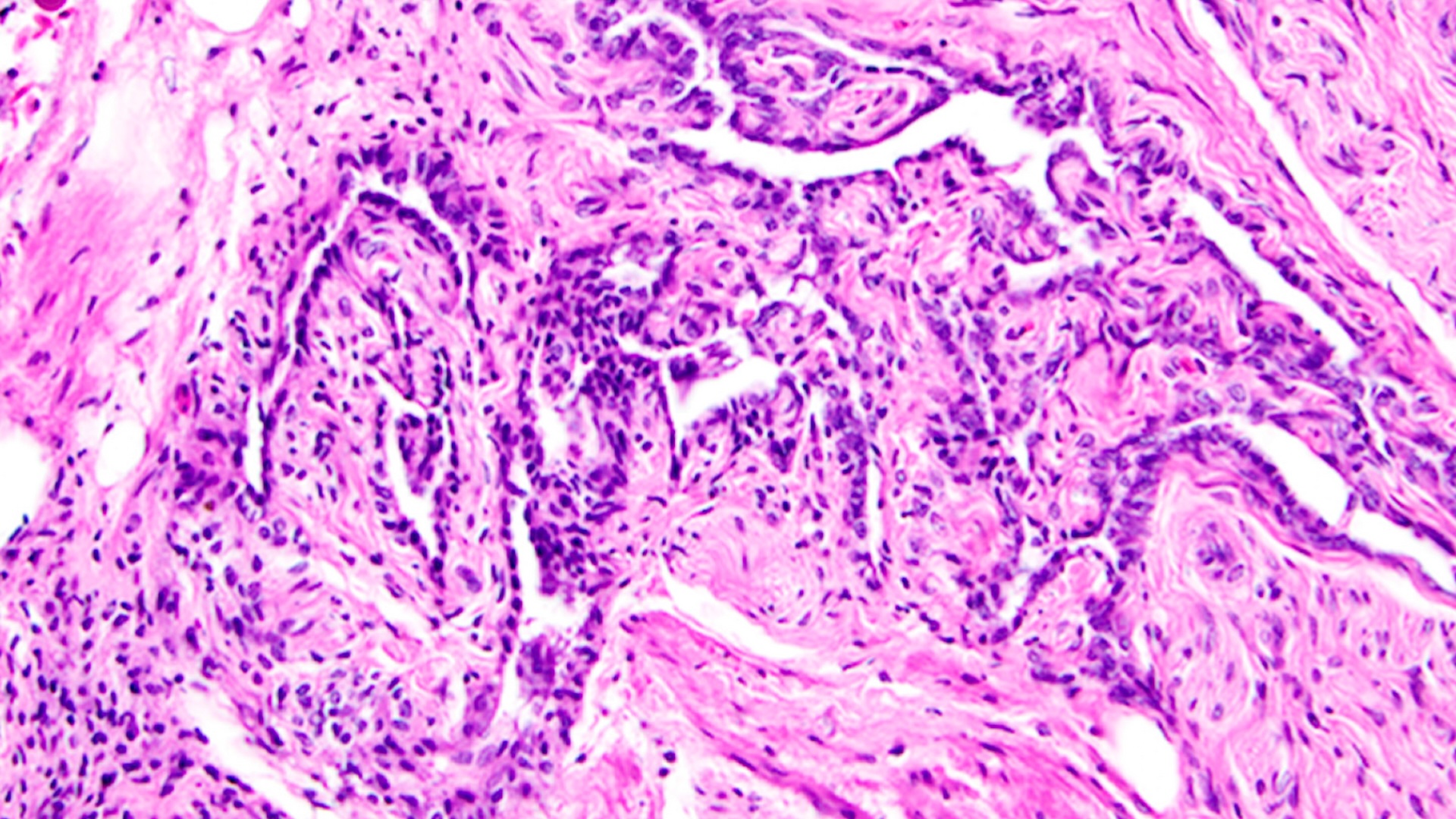
The virus and heart cells

When the coronavirus infects heart cells in a lab dish, the pathogen snips heart muscle fibers into tiny fragments, according to a new study. However, scientists don't yet know if the virus launches the same attack against the heart inside the human body.
Heart muscle cells, known as cardiomyocytes, are made up of small units called sarcomeres that line up end-to-end to form long, thin muscle fibers. But when exposed to SARS-CoV-2 in a lab dish, sarcomeres get sliced and diced into tiny bits. If this happened to a person's heart, it wouldn't be able to beat normally.
Related: The mysterious connection between the coronavirus and the heart
To see if the virus might behave similarly in the body, the study authors looked at autopsied heart tissue from three COVID-19 patients. They found that the sarcomere filaments from the patients were also disordered and rearranged, but not in exactly the same way as cells in the lab dish.
In both the lab dish experiments and autopsied tissue, some heart muscle cells appeared to be missing their DNA, which would effectively leave those cells "brain dead" and unable to function, the authors said. The scientists are now studying how the virus actually causes these changes in cells, whether they happen in the human body, and whether the damage can be prevented or reversed with medications.
Can the virus infect the brain?
Some people who catch COVID-19 develop disorientating neurological symptoms, like confusion, brain fog and delirium — now, a new study provides the first solid evidence that the virus might directly infect brain cells.
The study authors examined brain tissue from a patient who died of COVID-19, as well as two mouse models of the disease and clusters of brain cells in a lab dish, known as organoids. They found that the virus enters brain cells via the ACE2 receptor that sits on the cell surface. Lung tissue contains copious numbers of ACE2 receptors, and therefore many gateways for the virus to enter; the brain contains far fewer, but even so, the virus can still slip inside, the authors found.
Once inside, the coronavirus uses the internal machinery of brain cells to multiply, while also starving nearby cells of oxygen, which helps the virus reproduce. The researchers still need to determine how often the virus infects brain cells in patients with COVID-19, since some neurological symptoms may arise from elevated inflammation in the body and not directly from brain infection. In addition, we still don't know how the virus reaches the brain in the first place; the virus may pass through the barrier of tissue between the bloodstream and the brain, known as the blood-brain barrier, or enter through the nerves of the nose or eyes.
Originally published on Live Science.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.