FDA wants more proof COVID-19 plasma therapy works

The U.S. Food and Drug Administration (FDA) won't authorize the use of blood plasma to treat COVID-19 patients until more data about the treatment can be reviewed, federal officials announced.
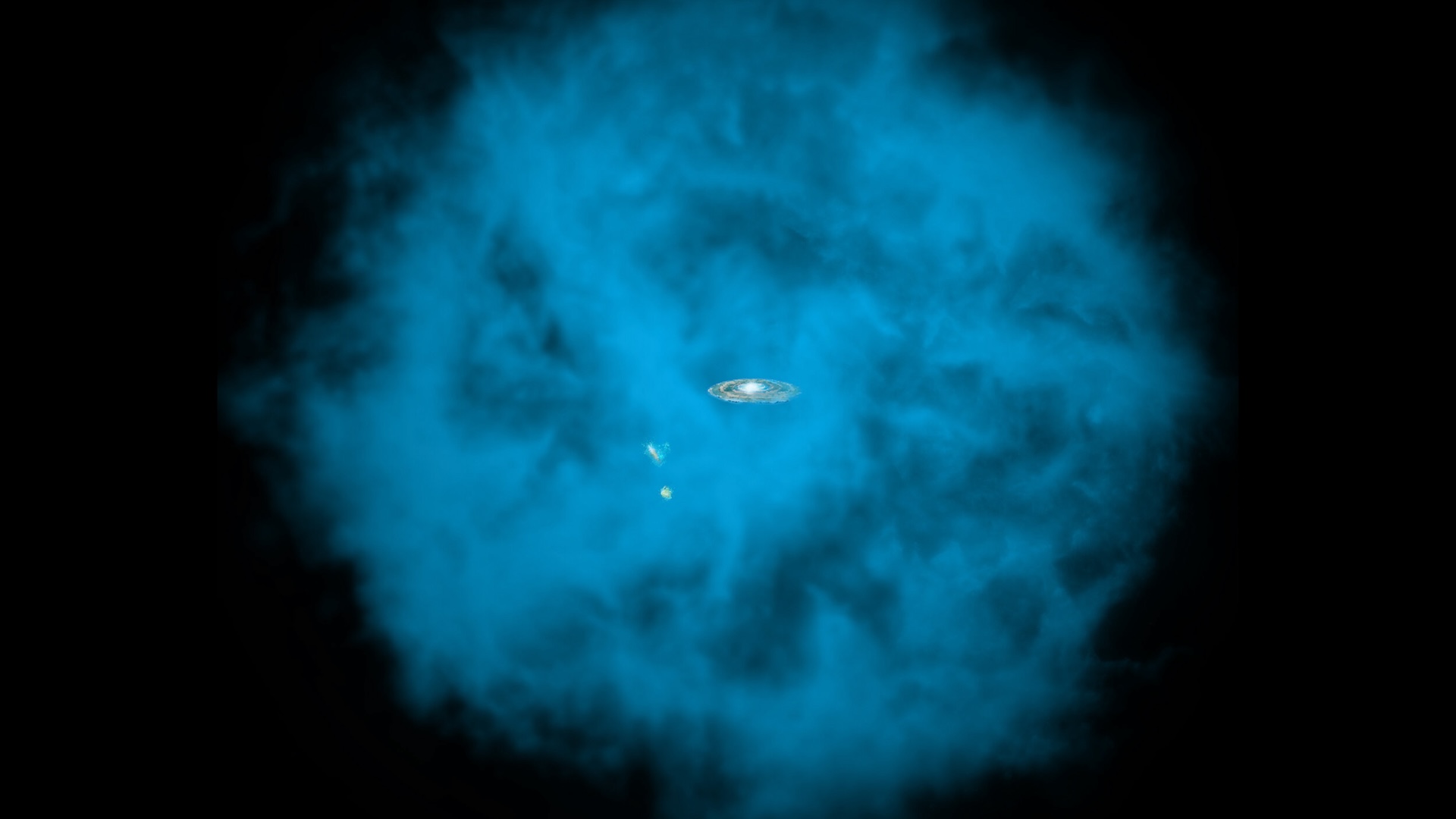
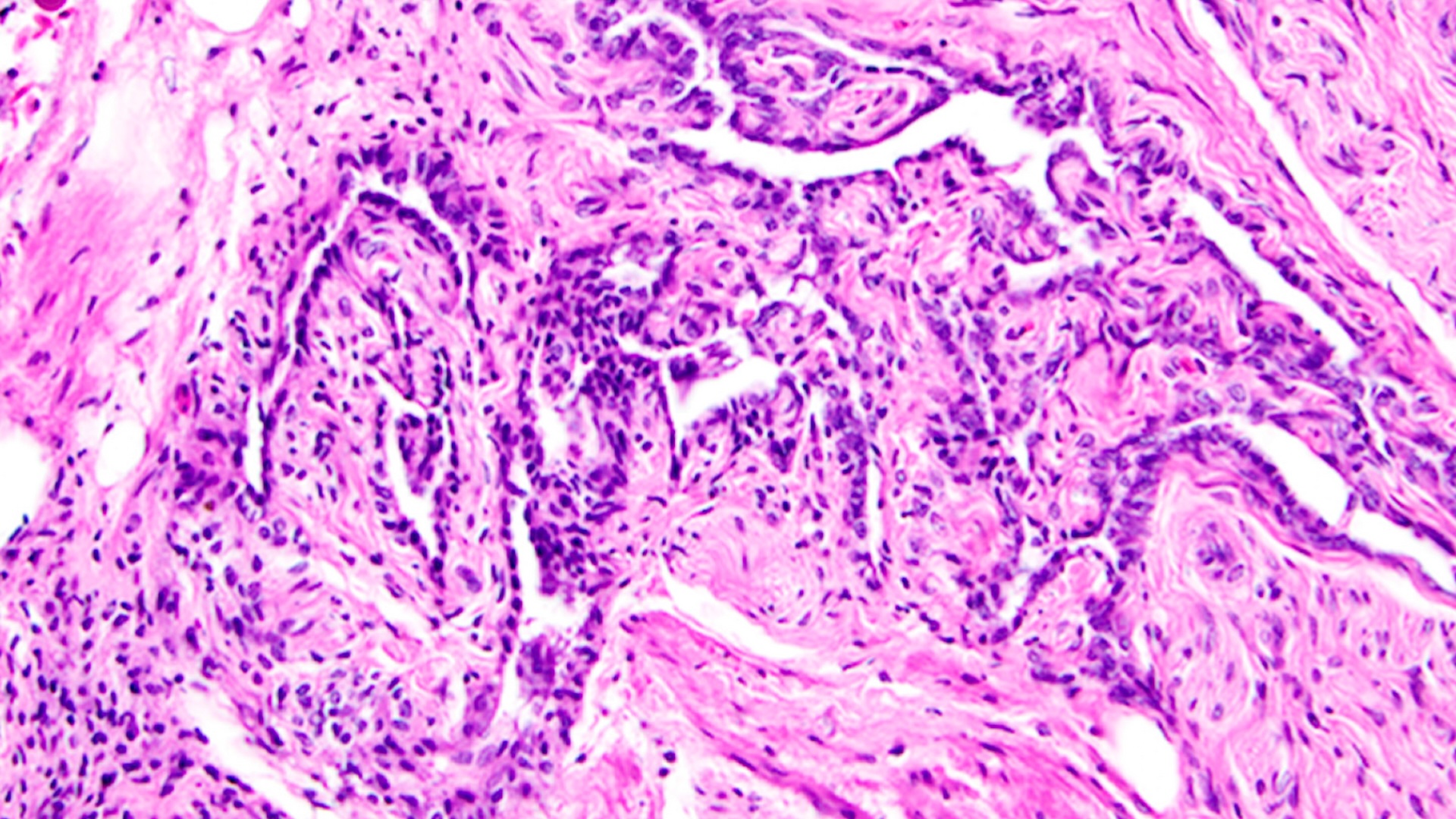
Convalescent plasma (CP) therapy relies on blood plasma donations from people who have recovered from an infectious disease, such as COVID-19, Live Science previously reported. The recovered person's blood contains antibodies that recognize the coronavirus, and in theory these molecules should help the immune system of a sick person take down the pathogen.
But no clinical trials have definitively shown that CP therapy helps coronavirus patients recover. Citing this lack of evidence, the country's top disease experts urged the FDA not to issue a so-called emergency use authorization for the therapy, The New York Times reported. Emergency authorization does not require the same degree of evidence as full FDA approval, but would allow doctors to widely apply CP therapy for COVID-19 "when there are no adequate, approved and available alternatives," according to the federal agency.
Right now, people receiving CP are doing so only through clinical trials. But because it is challenging to set up trials for CP, data showing whether it helps patients has been slow to come out. Authorizing the therapy too soon could make it even more difficult to gauge whether CP truly works, Dr. Mila Ortigoza, an infectious disease specialist at NYU Langone Health and co-leader of a clinical trial of CP therapy for COVID-19, told the Times.
Related: Treatments for COVID-19: Drugs being tested against the coronavirus
The FDA had already drafted an emergency use authorization form for CP therapy as of last week, but that process has now been put on hold after leading experts weighed in; these experts included Dr. Francis Collins, director of the National Institutes of Health (NIH), Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID) and Dr. H. Clifford Lane, NIAID clinical director.
"The three of us are pretty aligned on the importance of robust data through randomized control trials, and that a pandemic does not change that," Lane said in an interview Aug. 19, according to The New York Times. In a randomized controlled trial, or RCT, patients are randomly assigned to receive an experimental treatment or the standard of care, to see if the treatment works. "We want to make sure that when we say [CP therapy] works, we are confident, with indisputable evidence," Ortigoza told the Times. "We're dealing with patients' lives here," she said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Unfortunately, if history tells us anything, it's that it's exceedingly difficult to organize randomized trials for CP therapy, especially during a pandemic.
Doctors have studied convalescent plasma treatments since before the 1918 flu pandemic, and they also applied the therapy during the 2003 SARS outbreak, the 2009 H1N1 pandemic and the 2014 Ebola outbreak, Live Science previously reported. However, studies conducted during past viral outbreaks often lacked control groups, meaning patients who got CP therapy weren't compared to patients who didn't, to see if it truly improved outcomes. What's more, doctors can recruit patients for clinical trials only as they check into the hospital, and they can provide plasma only as donations become available.
Related: 20 of the worst epidemics and pandemics in history
Both study recruitment and plasma donations vary with the prevalence of COVID-19 in different regions, meaning that many clinical trials for CP often don't recruit enough participants to yield meaningful results — at least not quickly. In an effort to speed up the process and reach the necessary enrollment numbers, Ortigoza and others at NYU have organized an initiative to pool data from many ongoing randomized controlled trials of CP therapy.
"When evidence with a high degree of confidence emerges, the data and safety monitoring board will make a joint recommendation to the leadership of all trials," according to a statement on the initiative's website.
In the meantime, preliminary data from a dozen completed trials, including three very small RCTS, hint that COVID-19 patients treated with CP therapy die at significantly lower rates than those given standard treatments alone, according to a meta analysis posted July 30 to the preprint database bioRxiv. Additional data from the Mayo Clinic and Houston Methodist hospitals also hint at the therapy's safety and efficacy, but neither meet the standard of an RCT, according to the Times. A leader of the Mayo Clinic trial, Dr. R. Scott Wright, told the Times that plasma shortages and the need to organize the trial over conference calls has posed challenges.
"In a pandemic, you can't always get a definitive 'ah-ha' study" that clearly demonstrates a therapy's efficacy, Dr. Michael Joyner, an anesthesiologist and physician-researcher at the Mayo Clinic and author of the bioRxiv report, told Live Science in early August.
Lane of the NIAID said that the FDA could still grant emergency use authorization in the near future, barring more data from RCTs, the Times reported.
"We will keep going, because we're in desperate need of a randomized placebo-controlled trial for convalescent plasma," Ortigoza told the Times. "This is something our country and the world really needs right now."
Originally published on Live Science.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.