Alzheimer's comes in at least 5 distinct forms, study reveals
Knowing that Alzheimer's comes in at least five distinct forms could change the treatment landscape, the scientists behind the new study say.

Scientists have identified five subtypes of Alzheimer's disease, and they say the discovery represents the "first step" toward developing personalized treatments for the widespread condition.
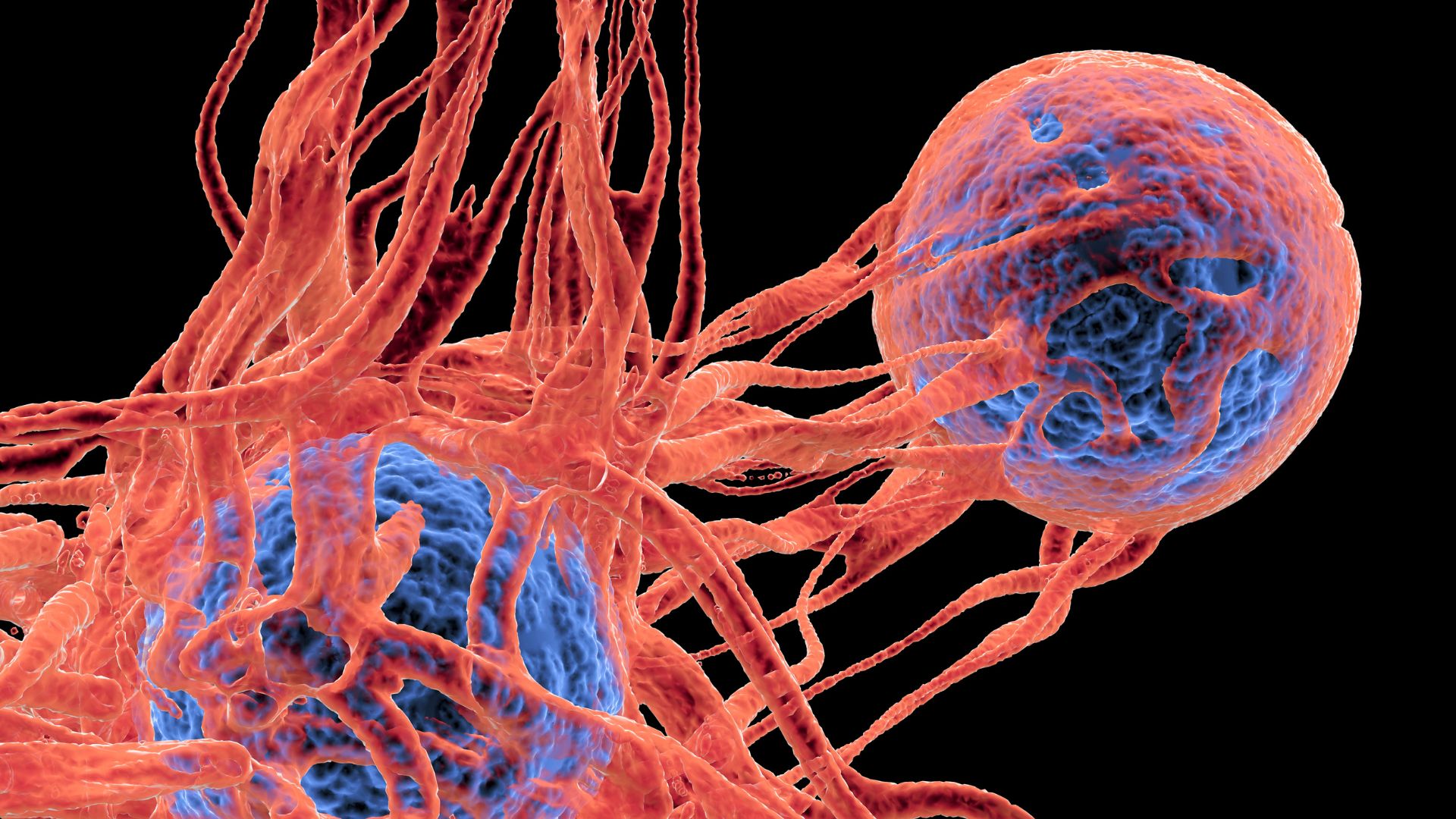
In a new study, scientists were able to sort more than 400 patients with Alzheimer's into five groups based on the levels of specific proteins in their cerebrospinal fluid (CSF), the clear liquid that surrounds the brain and spinal cord. These proteins are linked to biological processes that get derailed in Alzheimer's, such as the formation of new proteins and brain inflammation.
The five groups also displayed clear differences in their genetics and the clinical characteristics of their disease, such as the rate at which their symptoms progressed. The findings were published Jan. 9 in the journal Nature Aging.
Further work is needed to confirm that these newfound subtypes are relevant to how doctors treat individual patients with Alzheimer's, Bart De Strooper, a group leader at the U.K. Dementia Research Institute at University College London who was not involved in the research, told Live Science in an email. However, the findings are an "important step" toward being able to sort patients so that they receive the best drug for them at the right stage of their disease, he said.
Related: Europeans' ancient ancestors passed down genes tied to multiple sclerosis, Alzheimer's risk
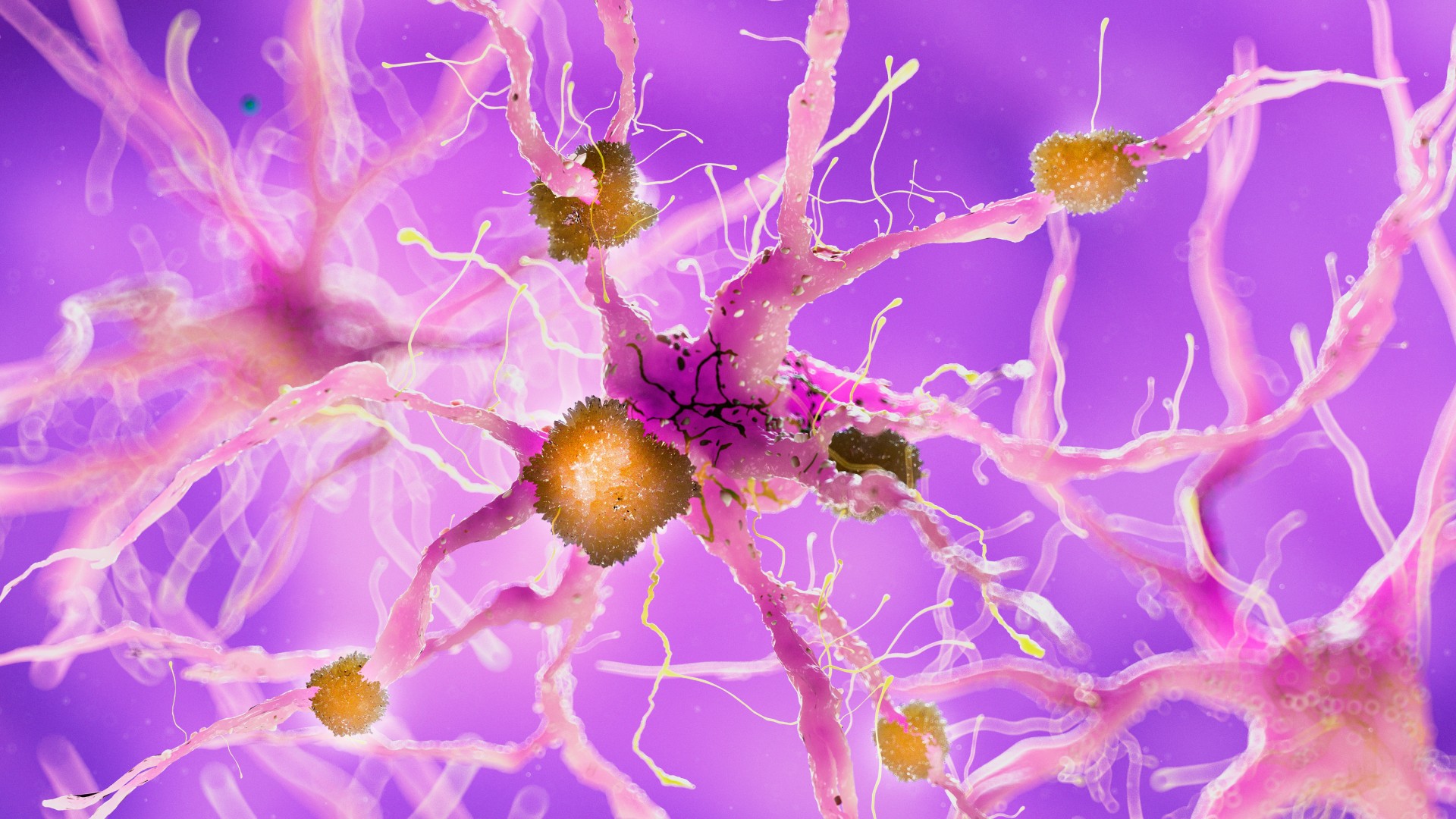
Alzheimer's disease is thought to be partially driven by a gradual buildup of amyloid-beta and tau proteins in the brain, which triggers a cascade of harmful processes that steadily kill brain cells. However, the specifics of this cascade vary from one person to the next which may explain why Alzheimer's drugs keep failing in clinical trials that don't consider this variability.
To try categorizing these differences between people, the study authors analyzed samples of CSF from 609 people who had been clinically assessed for dementia. They studied their CSF because it contains proteins produced by brain cells, and thus its contents can paint a picture of the biological processes occurring in the brain. Almost 70% of the group was diagnosed with Alzheimer's, which ranged in severity, while the remaining participants acted as a comparison group.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The authors identified 1,058 proteins that were found only in the CSF of patients with Alzheimer's. They then applied machine learning techniques — a type of artificial intelligence — to sort the patients according to the concentrations of these proteins.
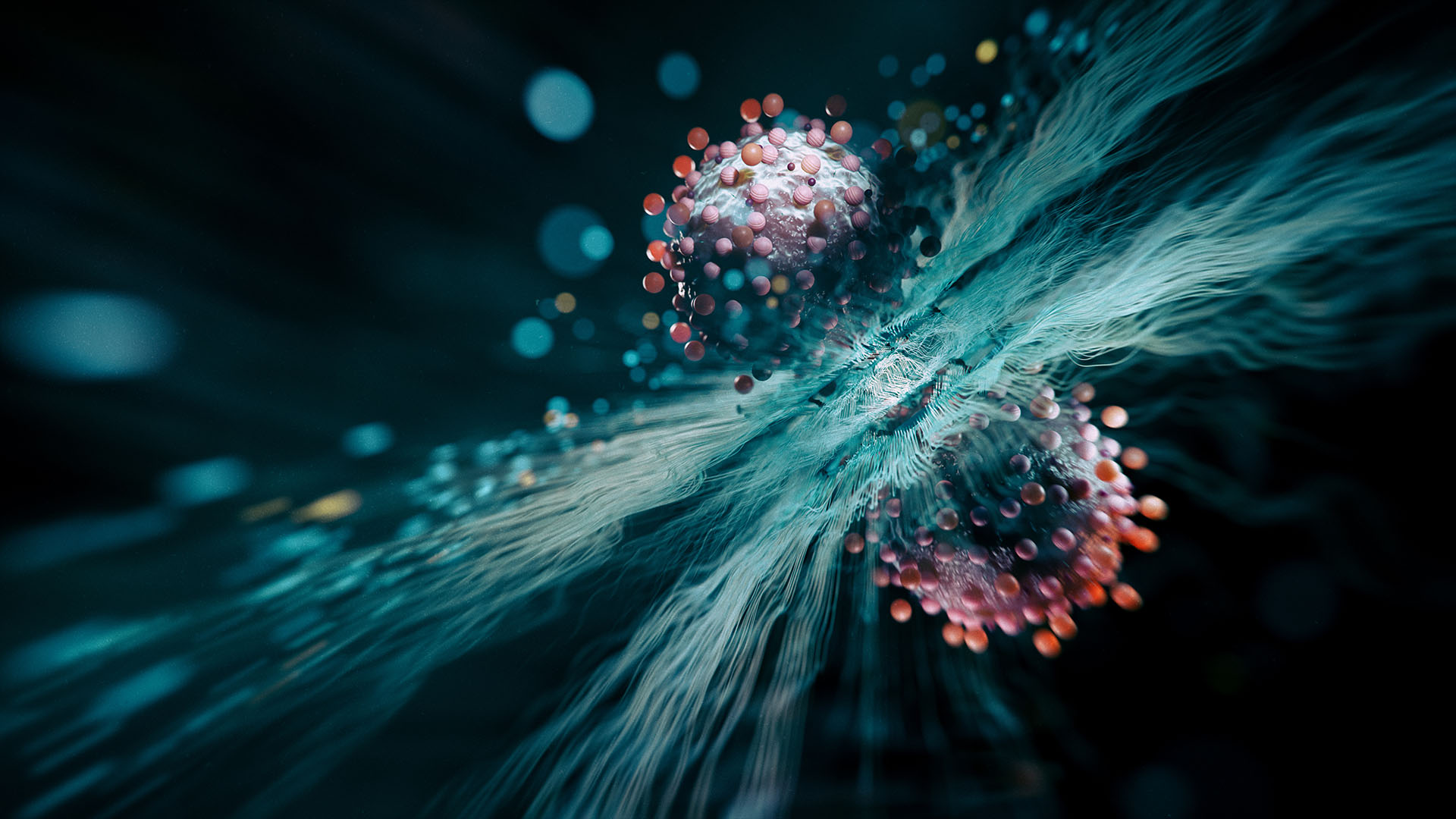
This revealed five distinct subgroups. People in one group, for instance, had more proteins linked to the dysregulation of RNA, a genetic cousin of DNA that's needed for protein synthesis, while others had more proteins involved in the activation of the immune system or in stimulating the growth of brain cells.
Related: Brain inflammation may drive mood changes in Alzheimer's
In a separate experiment, the authors looked at each patient's DNA and screened it for specific versions of genes, or gene variants, linked to Alzheimer's. They found that each subtype was tied to specific genetic variants that are associated with an increased risk of the condition. For example, patients in the neuronal-growth group were more likely to carry a gene variant linked to reduced activity in cells that usually help regulate cell growth.
Data on the participants' clinical symptoms and scans of their brains also revealed that each group's symptoms progressed at a different rate. In addition, their overall life spans varied, and they showed distinct patterns of brain-cell loss, in terms of where and how many cells died.
"I think this is really the first step towards personalized treatments," study first author Betty Tijms, an associate professor of neuroscience at Amsterdam UMC, told Live Science. Looking forward, trials testing new drugs for Alzheimer's could consider these subtypes when assessing the effectiveness of drugs and their side effects, she said. It may be that a given drug's mechanism works best for only one subgroup while causing unwanted side effects in another, for instance.
The study authors are also trying to get access to CSF samples from failed clinical trials, to see if the drug that was tested may have actually had subtype-specific effects.
And if they can conduct larger studies in the future, it could be possible for the team to detect more subtypes of Alzheimer's, Tijms suggested.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)