Brain inflammation may drive mood changes in Alzheimer's
Agitation, anxiety and depression seen in people with Alzheimer's may be driven by brain inflammation, in addition to abnormal proteins.
Extreme mood changes associated with Alzheimer's disease may be partially driven by brain inflammation, new research suggests.
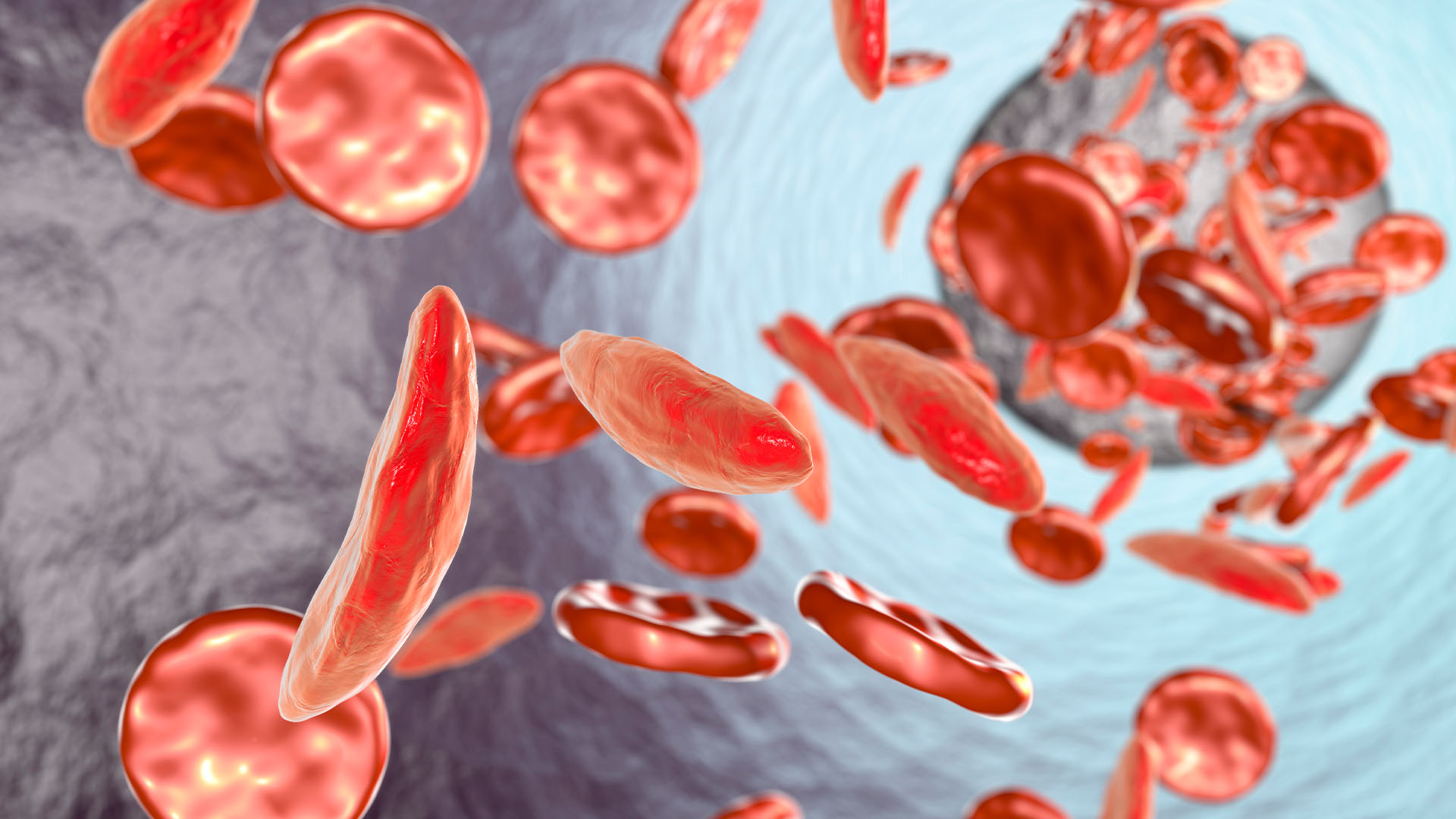
Historically, the prevailing theory for what causes Alzheimer's disease was that a gradual buildup of abnormal proteins called amyloid-beta and tau in the brain triggers a cascade of events, leading to nerve damage, the death of brain cells, and symptoms of cognitive decline and mood problems.
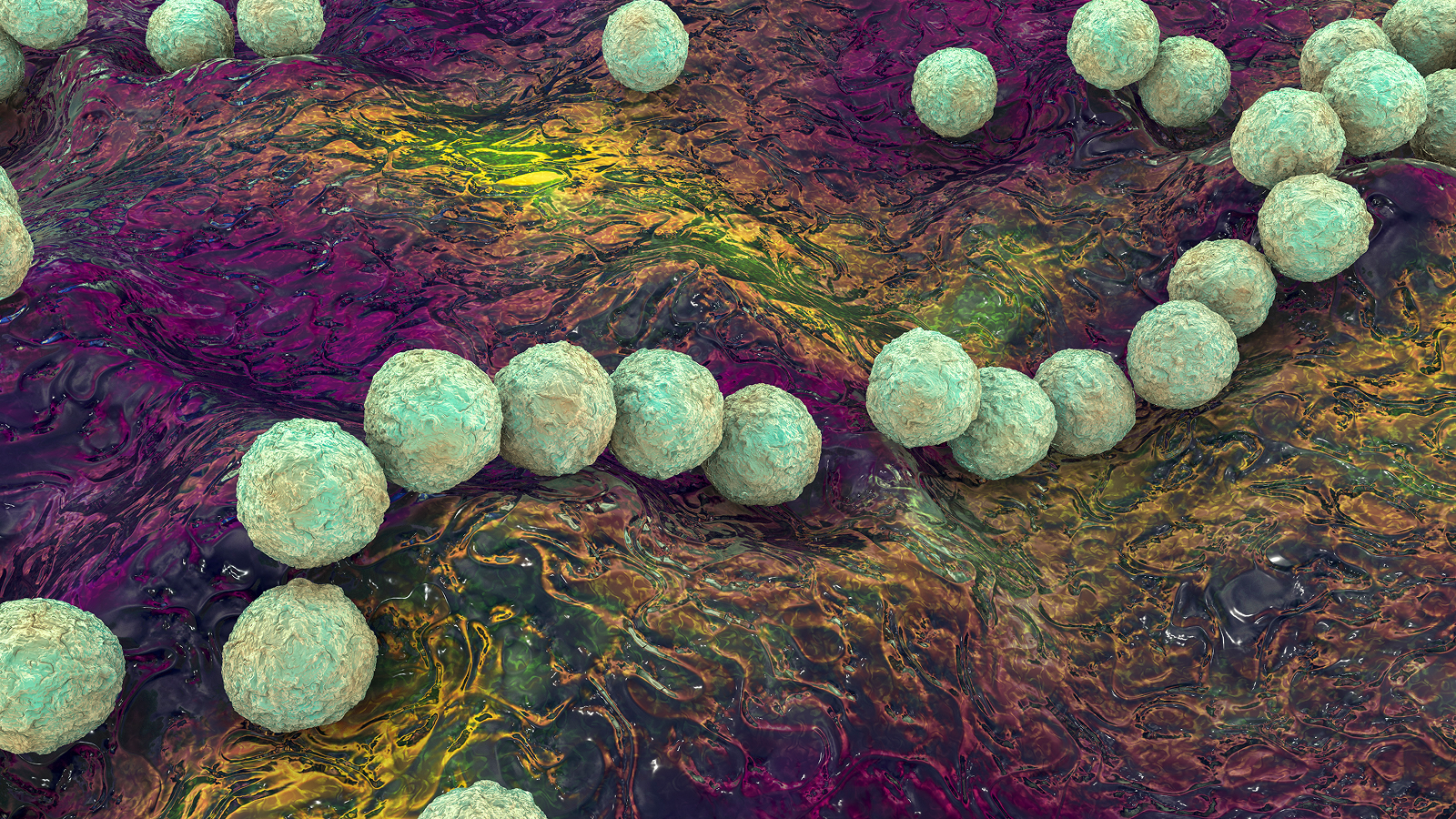
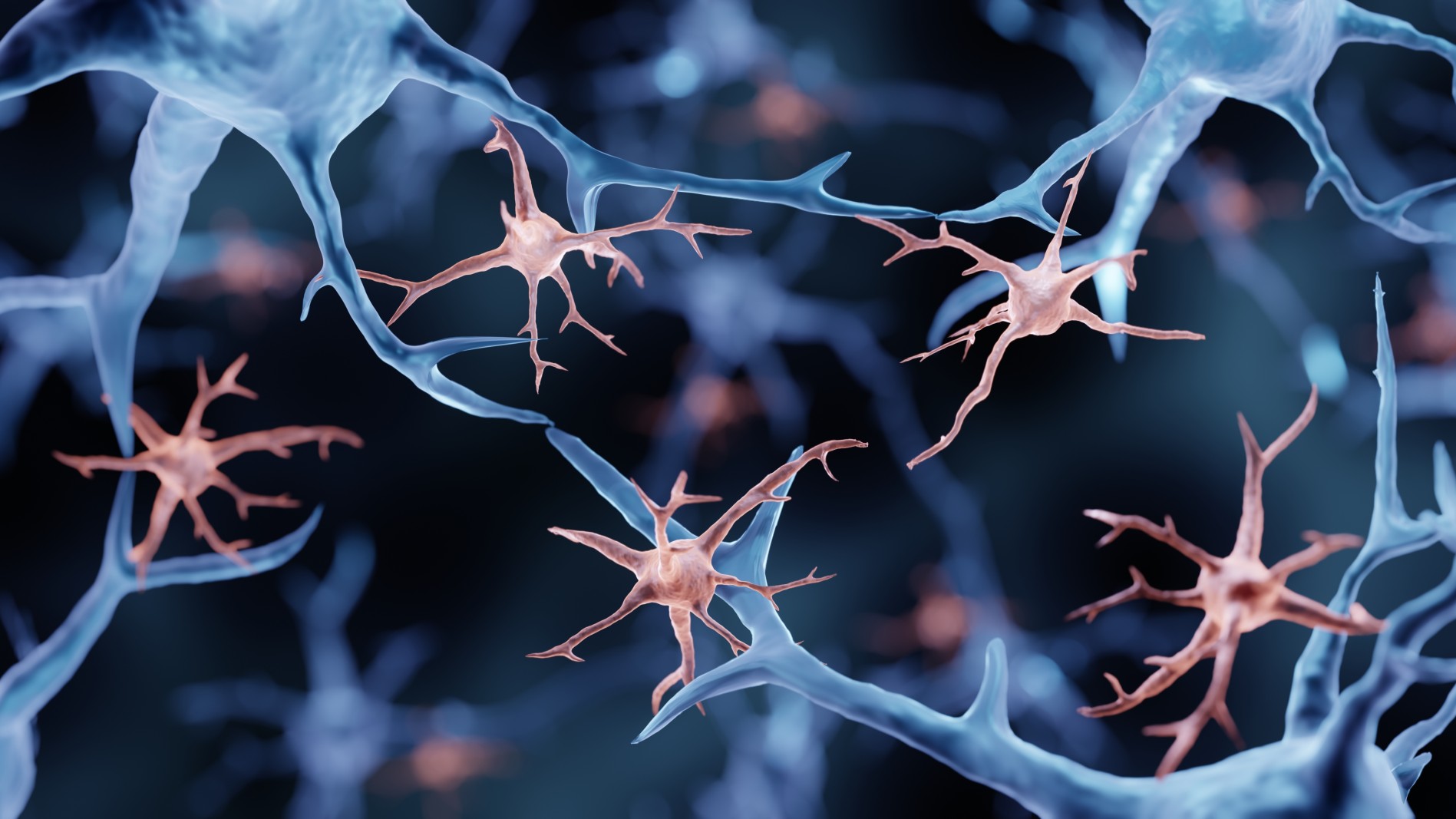
However, emerging evidence suggests that inflammation in the brain may also be involved in the development of the disease. Specific culprits include immune cells called microglia, which normally promote inflammation in response to injury or disease. Activated microglia have been found to interact with amyloid-beta and tau proteins and may influence the progression of Alzheimer's disease.
And now, in a study published Nov. 27 in the journal JAMA Network Open, scientists have provided what they say is the first strong evidence that the neuropsychiatric symptoms of Alzheimer's are directly associated with microglia activation.
Better understanding the role inflammation plays in the development of Alzheimer's could take us one step closer to developing more targeted treatments for the disease, the researchers say.
"Neuropsychiatric symptoms such as irritability, agitation, anxiety and depression are among the most difficult symptoms to treat in patients with Alzheimer's," Dr. Cristiano Aguzzoli, the study's lead author and a postdoctoral researcher at the University of Pittsburgh, said in a statement.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
"Here, we show for the first time that brain inflammation may be to blame for these symptoms," he said.
In the new study, the authors recruited 70 people who had no symptoms of cognitive decline and 39 who were cognitively impaired, either displaying early signs of memory loss known as mild cognitive impairment or dementia caused by Alzheimer's. The participants ranged from age 38 to 87.
The authors assessed whether the participants displayed any of the mood problems that are characteristic of Alzheimer's. The researchers also scanned the participants' brains to look for signs of microglial activation, as well as the accumulation of amyloid-beta and tau proteins.
People with cognitive impairment were more likely to have amyloid-beta and tau proteins in their brains. For example, amyloid-beta was found in 79% of those with cognitive impairment compared to 30% without.
However, even after taking these factors into account, the participants with more severe neuropsychiatric symptoms had a greater level of microglial activation and more substantial signs of inflammation than the participants with milder symptoms. This inflammation specifically affected three regions of the outer layer of the brain. Of the mood symptoms, irritability was most strongly associated with microglial activation, followed by nighttime disturbances and agitation.
The authors didn't directly compare whether participants' protein buildup was more or less strongly associated with mood problems than their inflammation levels. So they couldn't determine whether one factor is more influential than the other. However, the researchers think it's possible that both are playing a role.
In addition to conducting these tests, the researchers asked the caregivers of the patients with cognitive decline to fill out a questionnaire about their experiences. They found that the caregivers were more likely to report distress when looking after participants with greater levels of brain inflammation, particularly when it was linked to symptoms of irritability. Caregivers were also more likely to report that patients experienced rapid mood swings when the patients had high inflammation levels.
Going forward, the authors want to conduct more studies with larger groups of patients, including those who are at later stages of the disease and experience more extreme neuropsychiatric symptoms, such as hallucinations or delusions. This would assess whether the team's findings are more generalizable to the wider population of people with Alzheimer's.
In the meantime, they hope this research will act as a springboard for developing new therapies for Alzheimer's and possibly other types of dementia.
"Since both neuroinflammation and neuropsychological abnormalities are found in several other types of dementia, including Parkinson’s dementia, we are collaborating with scientists around the world to expand these findings to these other diseases," Dr. Tharick Pascoal, co-senior study author and an associate professor of psychiatry and neurology at the University of Pittsburgh, said in the statement.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)