New cells discovered in eye could help restore vision, scientists say
A new study suggests that never-seen-before stem cells in the human retina can restore vision in mice with a common eye disorder. But more work is needed to translate the treatment to people.

Scientists have identified never-before-seen cells in the human eye that could potentially help reverse vision loss caused by common diseases, such as macular degeneration.
The researchers discovered the cells in the retina, a light-sensitive structure at the back of the eye that is vital for vision. The cells were found in donated samples of fetal tissue.
The scientists also identified the same cells in lab-grown models of the human retina — and when they tried transplanting those models into mice with a common eye disorder, it restored the rodents' vision.
"This research not only deepens our understanding of retinal biology but also holds immense potential for advancing therapeutic interventions in RD [retinal degeneration] diseases," the researchers wrote in a paper describing the findings, which was published March 26 in the journal Science Translational Medicine.
Related: Scientists restore monkey's vision with a patch made from human stem cells
The retina detects light and converts it into signals that the brain can then interpret to determine what we're seeing. Deterioration of the retina is a leading cause of blindness worldwide. It can be triggered by many things, including aging, diabetes and physical injury, and the degeneration can lead to common eye diseases, such as macular degeneration and retinitis pigmentosa.
Current treatments for these conditions focus mainly on reducing the rate at which retinal cells deteriorate, and protecting those that are still healthy. However, there are currently no effective therapies that promote repair of the retina, which would effectively reverse the deterioration.
Get the world’s most fascinating discoveries delivered straight to your inbox.
A potential solution is to replace deteriorated cells with stem cells — cells that can mature to become any type of cell in the body under the right conditions. Yet, until now, scientists haven't found suitable stem cells in the human retina to achieve this, the authors of the new study wrote.
In the new research, the team analyzed the activity of cells in the fetal retinal samples in the lab. The scientists discovered two types of retinal stem cells with promising regenerative properties: human neural retinal stem-like cells (hNRSCs) and retinal pigment epithelium (RPE) stem-like cells.
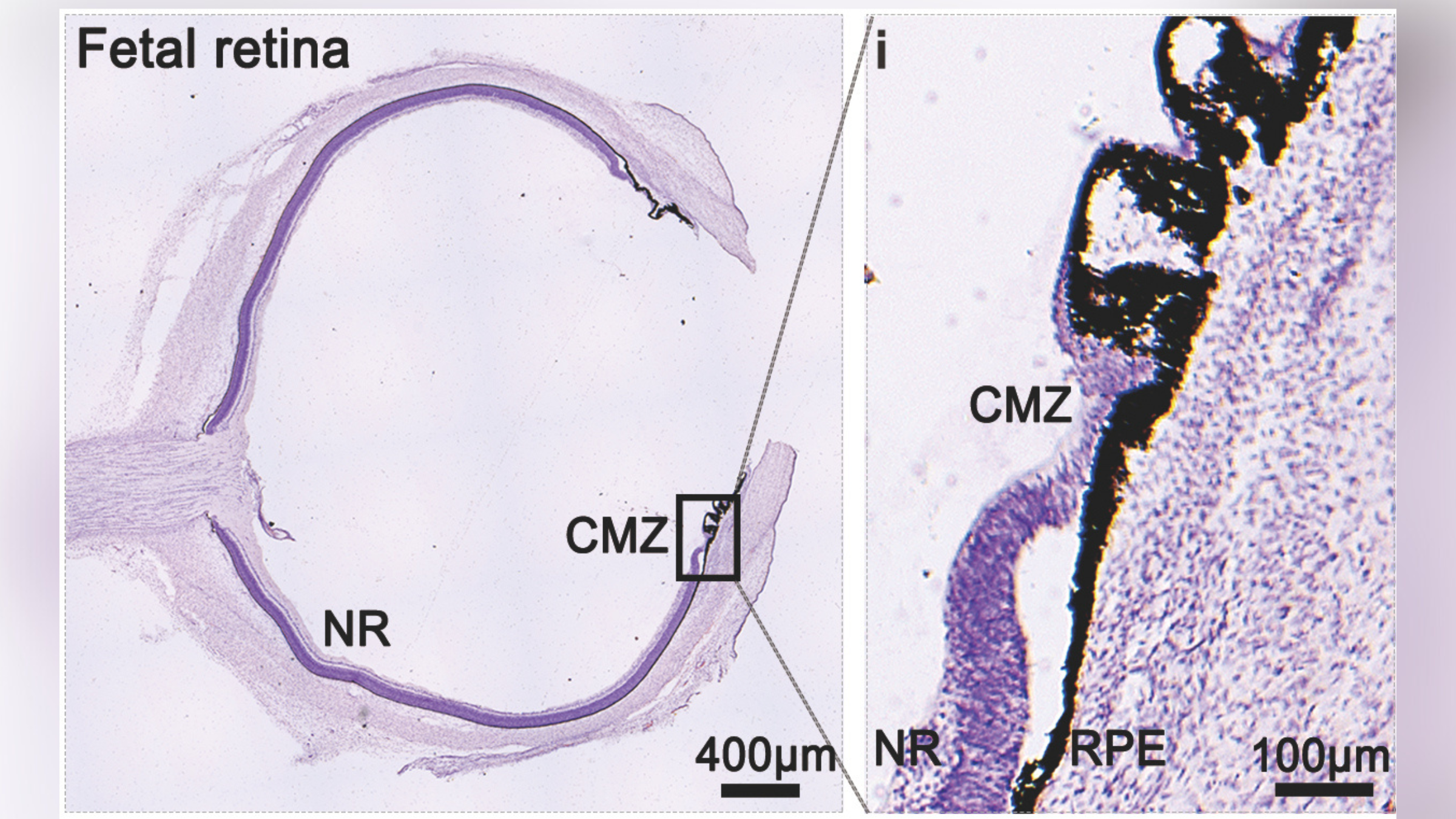
The researchers found that both types of cells, which were located in the outer edge of the retina, could clone themselves. However, only hNRSCs could turn into other types of retinal cells under the right conditions.
In a separate experiment, the researchers grew miniature replicas of the human retina in petri dishes. These 3D tissue models, known as organoids, better mimic the unique complexities of human organs than traditional animal models do.
An analysis of the cells within these organoids revealed that they contained hNRSCs similar to those found in the fetal tissue samples. The team also identified specific molecular chains of events that turned the stem cells into other retinal cells and regulated the repair process.
When transplanted into the retina of mice with a disease similar to retinitis pigmentosa, the stem cells from the organoids turned into the retinal cells needed to detect and process light signals. These new retinal cells ultimately improved the vision of the mice, compared with rodents that didn't receive any transplanted cells. This effect was seen for the duration of the experiment, up to 24 weeks.
Taken together, these early findings suggest that hNRSCs could be used to develop new treatments for retinal eye disorders in humans. But more research will be needed to confirm the potential of these cells for restoring the vision of human beings.

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.


