COVID drug molnupiravir may be driving the virus to mutate — should we worry?
The antiviral molnupiravir may be shaping the evolution of the virus behind COVID-19, but we still don't know what this means for transmission or the emergence of variants.

An antiviral drug used to treat COVID-19 may be driving the virus that causes the disease to evolve, a new study suggests.
But is this concerning, or particularly surprising? Not at this point, and not really, experts told Live Science.
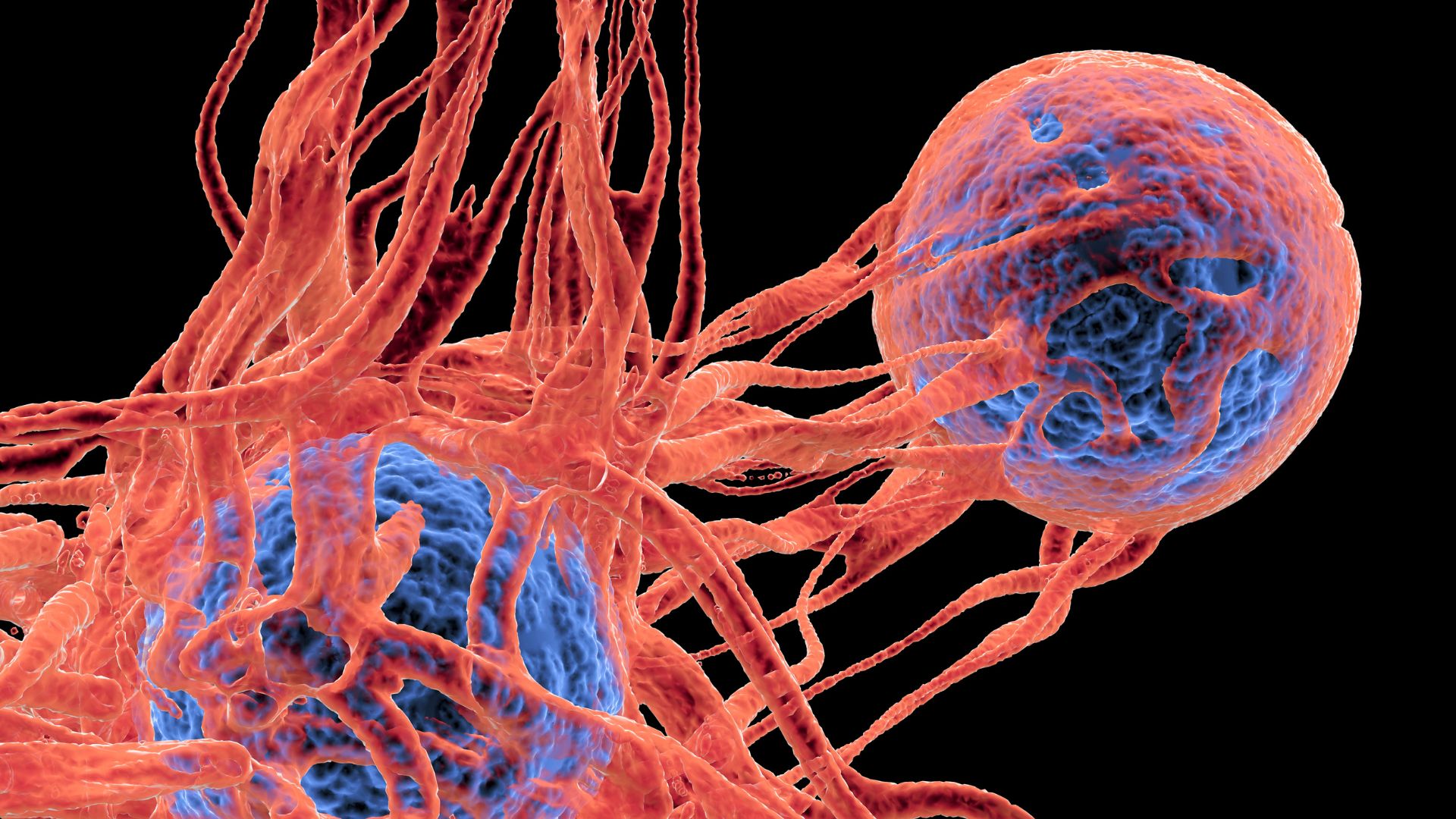
Scientists analyzed more than 15 million SARS-CoV-2 genomes — genetic material from the virus that causes COVID-19 — and found that molnupiravir induces a "mutational signature" that, if the virus isn't completely obliterated by a course of the drug, can be transmitted to other people. Molnupirivar works by causing mutations in the SARS-CoV-2 genome that prevent the virus from replicating.
"Previously people had raised the mutagenic effect of molnupiravir on viruses as a theoretical risk," study lead author Theo Sanderson, a researcher at the Francis Crick Institute in London, told Live Science in an email. "Our work makes this more concrete because we have found that molnupiravir can give rise to extensively-mutated viruses that remain transmissible," he said. What's more, some of the mutations that cropped up repeatedly seem to be ones that could help the virus evade the immune system, he added.
Related: New antiviral pill halves risk of COVID-19 hospitalization, Merck says
The authors of the study, published Monday (Sept. 25) in the journal Nature, found that after molnupiravir's rollout, this mutational signature was common in countries that widely used the drug, such as the U.S. and U.K. However, countries where molnupiravir is not licensed, such as Canada, had fewer examples of these signatures.
The findings could help regulators to assess the risks and benefits of using the drug, but experts told Live Science that many questions remain unanswered.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.

"We should not be concerned with mutations themselves, but rather whether they allow the virus to adapt to infect or transmit better," said Vaughn Cooper, a professor of microbiology and molecular genetics at the University of Pittsburgh who was not involved in the research. "In this case, we see relatively little evidence that molnupiravir is fueling more adaptations to escape prior immunity or alter infectiousness," Cooper told Live Science in an email.
Indeed, Sanderson said from this data alone, it is difficult to quantify how common it is for molnupiravir-derived lineages of SARS-CoV-2 to spread between people. That's because, if a single sample of the virus with this molnupiravir signature shows up in a database but doesn't have any close relatives, scientists can't easily tell if it came from someone treated with the drug or another person infected further down the line.
The study also didn't address the potential risks and benefits of using molnupiravir for individual patients, Sanderson said. This will be important to understand, especially for those with weakened immune systems, he said. These patients have a higher risk of prolonged COVID-19 infections that give the virus more opportunities to pick up lots of mutations.
Future modeling studies could help predict whether the drug could influence the risk of new variants of concern emerging — another question that the current study didn't explore, Sanderson added.
"We have yet to see evidence of more fit sequences arising from molnupiravir" — meaning viruses that can more easily spread and multiply — "but this work certainly provides pause for thought and should weigh heavily in considerations around future use of the drug, necessitating at the very least mitigations of the risks of this effect, alongside real world data on the effectiveness of the drug," Aris Katzourakis, a professor of evolution and genomics at the University of Oxford who was not involved in the research, told Live Science in an email.
Mitigation strategies could include selective prescribing and monitoring chronically infected patients for evidence of viral evolution, but these safeguards would need to be balanced against patients' clinical needs and the availability of alternative treatments, he said.
This article is for informational purposes only and is not meant to offer medical advice.

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)