Endometriosis may quadruple risk of ovarian cancer, study finds
Women with severe endometriosis are 10 times more likely to get ovarian cancer, while people with endometriosis of any severity are four times as likely, a study suggests. But patients shouldn't panic.

Women with endometriosis may have a substantially increased risk of ovarian cancer, new research suggests.
In the study, women with endometriosis were more than four times as likely to get ovarian cancer than those who did not have the disease. For women with severe endometriosis, the risk of cancer jumped nearly tenfold.
However, experts cautioned that this still represents a relatively small increase in risk, overall, and that patients with endometriosis shouldn't be unduly concerned.
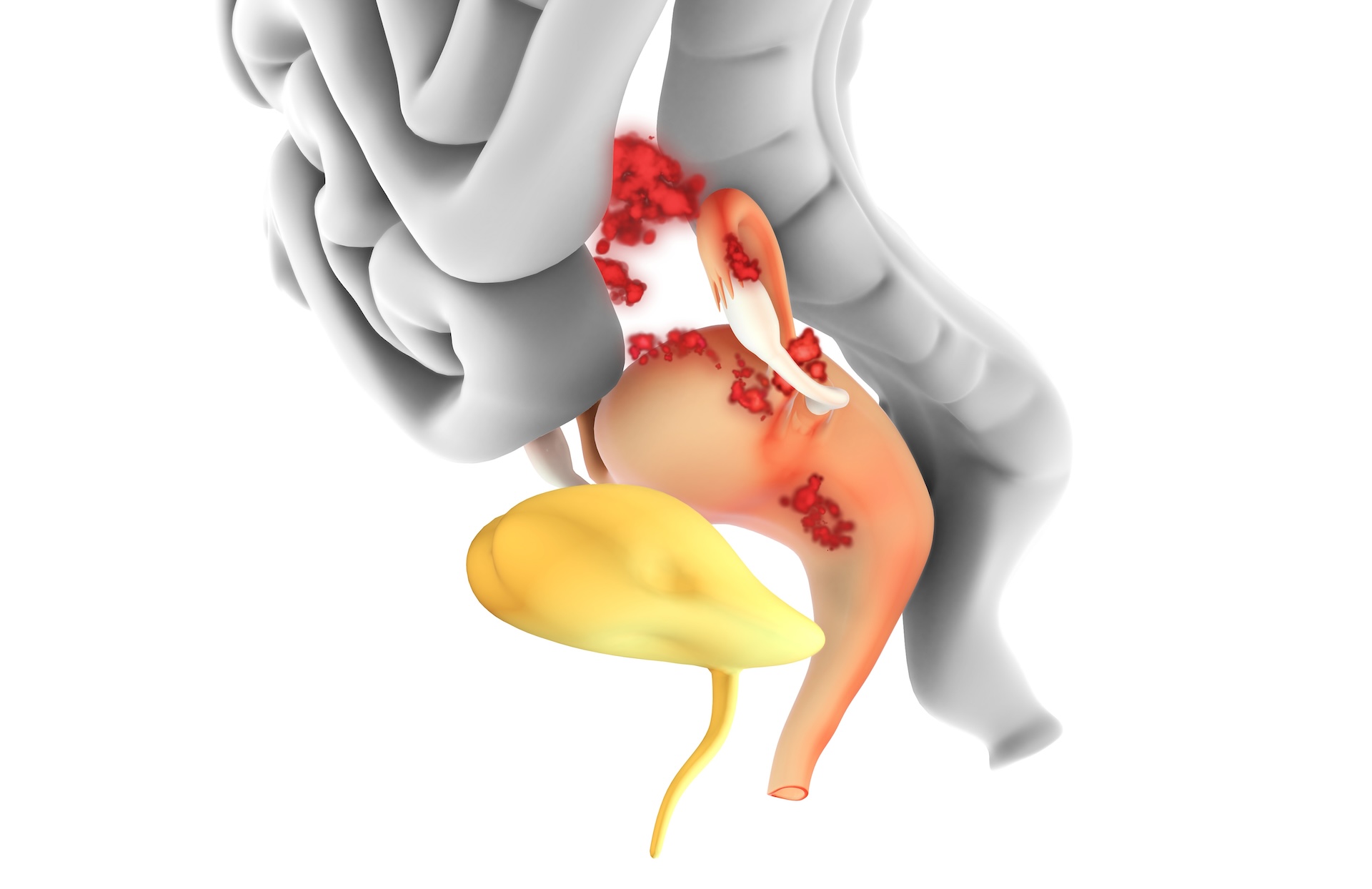
The study, published July 17 in the journal JAMA, included nearly 78,900 U.S. women with endometriosis. The disease, which affects approximately 10% of reproductive-age women, occurs when tissue similar to the lining of the uterus starts growing outside the organ, triggering inflammation and scarring.
Related: Why is endometriosis so hard to diagnose?
There are different types of endometriosis, which vary depending on whether the wayward tissue grows on the membrane that covers organs in the pelvis, in the ovaries, or on and between other organs in the pelvic and abdominal regions. These types vary in their severity, but in general, endometriosis is strongly associated with pelvic pain, infertility, irritable bowel syndrome, and breast, endometrial and ovarian cancers.
Previously, a study from Finland reported that women with endometriosis had double the chance of getting ovarian cancer and 10 times the risk if they had the form of the disease that affects the ovaries, compared with those without the condition. However, that study lacked enough samples to conduct a detailed analysis of the risks tied to each type of endometriosis.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The new JAMA study fills that gap.
"I am passionate about giving women quantitative information that can help them in shared decision making with their primary care providers or gynecological care providers," study co-author Karen Schliep, a reproductive and perinatal epidemiologist at the University of Utah, told Live Science.
At this point, the study doesn't point to any changes in who should get diagnostic or preventive surgeries for ovarian cancer, Schliep stressed. However, "my hope is that, working with other researchers and particularly cancer experts, we can look at development of prediction models that can be used by clinicians and their patients for helping to make some of these tough decisions," she said.
For the study, Schliep and her colleagues pulled information on women ages 18 to 55 from the Utah Population Database. The final cohort included 78,893 women with a history of endometriosis and about 379,000 women without known endometriosis. Within those groups, it included nearly 600 women with ovarian cancer.
The authors split endometriosis into five categories, depending on which organs it affected, and they split the ovarian cancers into two types, based on whether they grew locally or more aggressively.
This large dataset revealed that the women with any type of endometriosis had a 4.2-times-higher lifetime risk of developing ovarian cancer, compared with women without the condition. In this overall group, the boost in risk was higher for local cancers than for aggressive cancers.
For those whose condition affected only the pelvic organs, the cancer risk was 19 times higher than baseline. Those confirmed to have endometriosis on both their pelvic organs and ovaries simultaneously had a 13-times-higher risk. Again, the risk of local cancers was higher than that of aggressive cancers, although both risks were elevated.
Related: New blood test detects ovarian cancer years before conventional methods
"It is of interest to determine — and we don't have a way of doing this right now — which are those few people that have endometriosis and are at higher risk of ovarian cancer," said Dr. Paul Yong, a gynecologist and researcher at the BC Women's Centre for Pelvic Pain & Endometriosis who was not involved in the study. "And then how do you identify them ahead of time? How do you prevent it?"
The size of the study is a strength, but it does have limitations. It's possible that some cases of endometriosis and ovarian cancer may be misclassified as the wrong subtypes, and there was also a lack of data on the use of hormonal contraceptives, some of which are known to reduce the risk of ovarian cancer.
"At the moment, at least on the data that's been presented, the message shouldn't be that there's this hugely increased ovarian cancer risk amongst women with endometriosis, because we simply do not have the evidence that that's the case," said Krina Zondervan, a reproductive and genomic epidemiologist at the University of Oxford who was not involved in the study.
Zondervan emphasized that women with endometriosis should not be unduly concerned and jump to having their ovaries removed. This brings on premature menopause that can raise the risk of other conditions, such as cardiovascular disease and osteoporosis, she noted.
Data suggest that very few women with endometriosis get ovarian cancer — the lifetime risk of ovarian cancer for women without endometriosis is 1.3%, and prior to this study, the reported risk for women with endometriosis was 1.8%. The new analysis raises this risk by only 0.1% — or about 10 extra cases per 10,000 people with any type of endometriosis. That still puts the overall risk much lower than the general population's risk of developing breast (13%), lung (6%) or bowel (4%) cancer.
Nonetheless, "if a patient comes with concern about risk of ovarian cancer, I think they should be validated," Yong said. "The clinician should talk about it with the patient and not ignore it."
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Sahana Sitaraman is a science writer based in Lausanne, Switzerland, specializing in biology. She particularly enjoys writing about unusual animal behaviours and the neuroscience behind them, mental health and women in STEM. She also dabbles in illustrating cool findings that pique her interest. In her free time, Sahana can be found out on a hike, acting it up with the local improv group or painting. She holds a bachelor's degree in microbiology from the University of Delhi, India and a master's and PhD in life sciences from the National Centre for Biological Sciences in Bangalore, India.









