Massive study of 3 million people reveals genetic 'hotspots' linked to bipolar disorder
A new study has greatly expanded the number of gene variants thought to be tied to bipolar disorder.
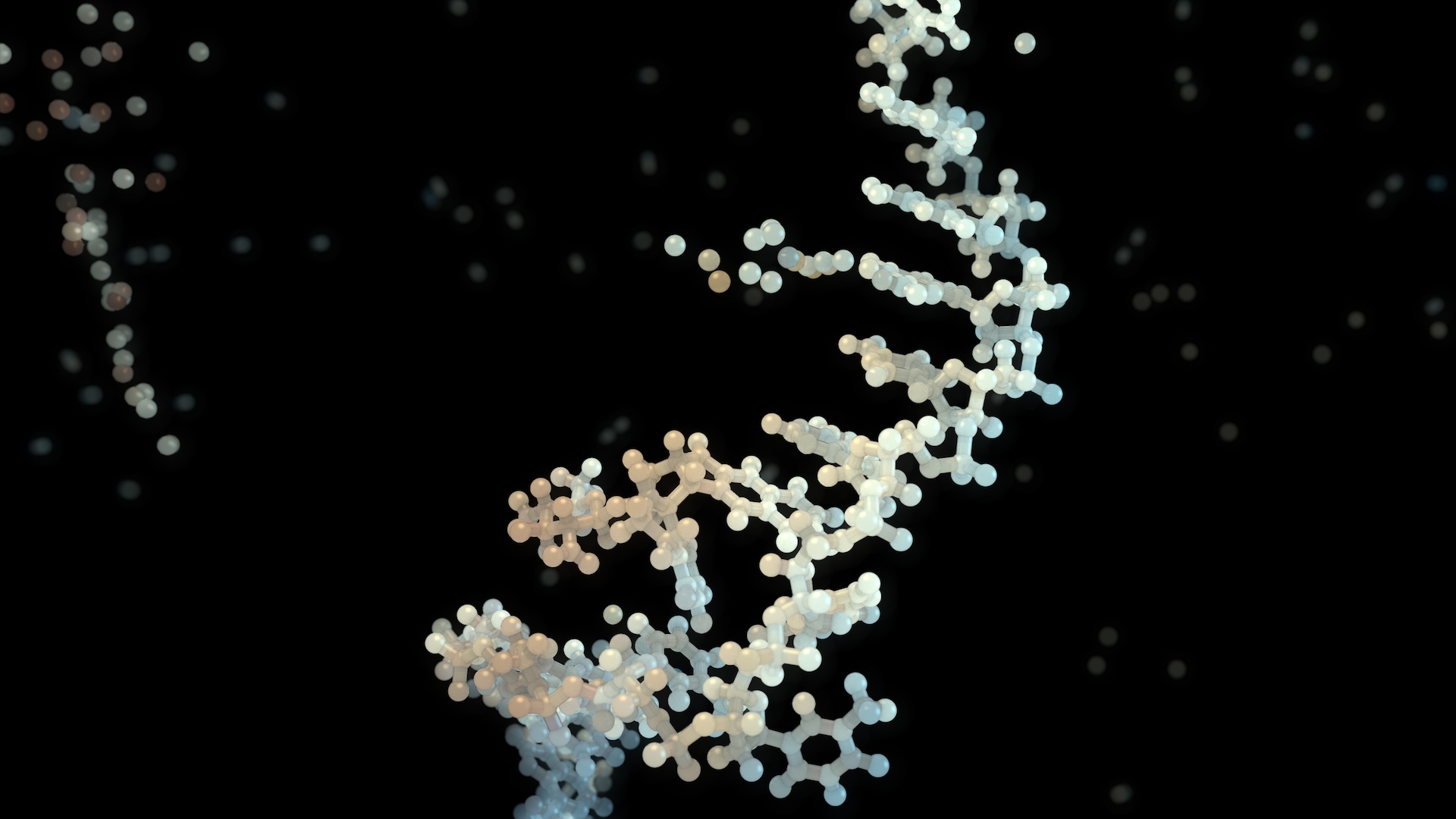
Scientists have pinpointed nearly 300 "hotspots" in the human genome that may increase the risk of bipolar disorder.
In the largest study of its kind to date, an international research team conducted a thorough analysis of DNA from almost 3 million individuals, including more than 158,000 with bipolar disorder. The DNA data was collected from people of European, East Asian, African and Latino descent, located in 27 countries.
In this trove of genetic information, the researchers identified 298 stretches of the genome containing gene variants that may boost the risk of bipolar disorder. They also zoomed in on 36 specific genes linked to the disorder.
Of those 36 genes, 16 are known to be targets of small molecules that could potentially be used as drugs to tweak the genes' activity, first study author Kevin Sean O'Connell, a researcher at the University of Oslo's Center for Precision Psychiatry, told Live Science in an email. "This indicates potential for novel drug development but further research in pharmacological aspects is required that was beyond the scope of this work." The new study was published Jan. 22 in the journal Nature.
Related: PTSD tied to 95 'risk hotspots' in the genome
Exploring the genetic landscape of bipolar
Bipolar disorder (BD) is a psychiatric condition characterized by extreme shifts in mood and energy, including euphoric states, or manic episodes; and hopeless states, called depressive episodes. People can also experience symptoms of mania and depression in mixed episodes. There are two main types of BD, including bipolar I — which cycles between longer bouts of depression and mania — and bipolar II, which involves depression and "hypomania," a less extreme state.
BD affects nearly 1 in 150 adults worldwide, but its biological basis is not well understood. Evidence suggests genetics plays a big role, and specific gene variants have been tied to the disorder in the past. However, most of that past research was conducted in people of European ancestry.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
By incorporating people from many backgrounds, the scientists uncovered genetic traits that were common across several demographics, as well as unique traits seen only in specific demographics.
"We identified an East Asian ancestry specific locus that is associated with the disorder," O'Connell said. "This particular variant is not present in individuals of European or African American ancestry. It will be interesting to determine how this variant might influence risk."
"Still," he clarified, "most of the variants show signals across the different ancestries."
The new study also increased the number of genomic regions tied to BD by fourfold, compared with previous studies. But one commonality between past studies and this new one is that they provide "biological evidence" supporting lithium as a BD treatment, O'Connell said. Two of the 36 genes the team identified are "lithium target genes," he explained. Future investigations could help unpack how genes' functions and their response to the drug.
Lithium has long been used as a mood stabilizer in the treatment of BD, but how it works is not well understood, so this line of research might provide some hints. Notably, though, lithium can cause a range of side effects, so scientists are looking for new solutions to treat the disorder.
There are some second-generation antipsychotics approved for bipolar that sidestep some of the problems associated with lithium, said Chaya Bhuvaneswar, a psychiatrist, writer and medical director of the North Suffolk Mental Health Association, who was not involved in the study. "However, these antipsychotics have their own set of issues," including the potential to raise the risk of type 2 diabetes, she told Live Science in an email.
The new study could be a starting point to uncover new clinical approaches for BD, the study authors wrote in their report. For instance, the results hint that there may be distinct genetic differences between people with BD I and BD II. The team flagged this potential difference between their participants who'd been recruited through hospitals or large population studies and participants who'd filled out online health surveys. The former group was more likely to have BD I while the latter had higher rates of BD II.
This "wouldn't be the type of genome-wide observation that one could notice in (far smaller) clinical samples," Bhuvaneswar said.
The study also pointed to specific cells tied to BD. For instance, it flagged clusters of genes known to be active in GABAergic interneurons — key nodes in brain circuits that tamp down the activity of neurons they're linked up to. Neurons in the pancreas and intestine were also implicated, but more research is needed to confirm how these are related to BD.
"What I would read from this study," Bhuvaneswar said, "is that there is increasingly robust evidence of genetic determinants of bipolar disorder."

Sibani Ram is a recent graduate of Duke University, originally from Iowa City, Iowa. She is passionate about medicine, journalism and entrepreneurship. Her work has previously also been published in The Los Angeles Times and The Boston Globe.
- Nicoletta LaneseChannel Editor, Health
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.