The rare genetic disorder that causes severe itchiness and liver failure
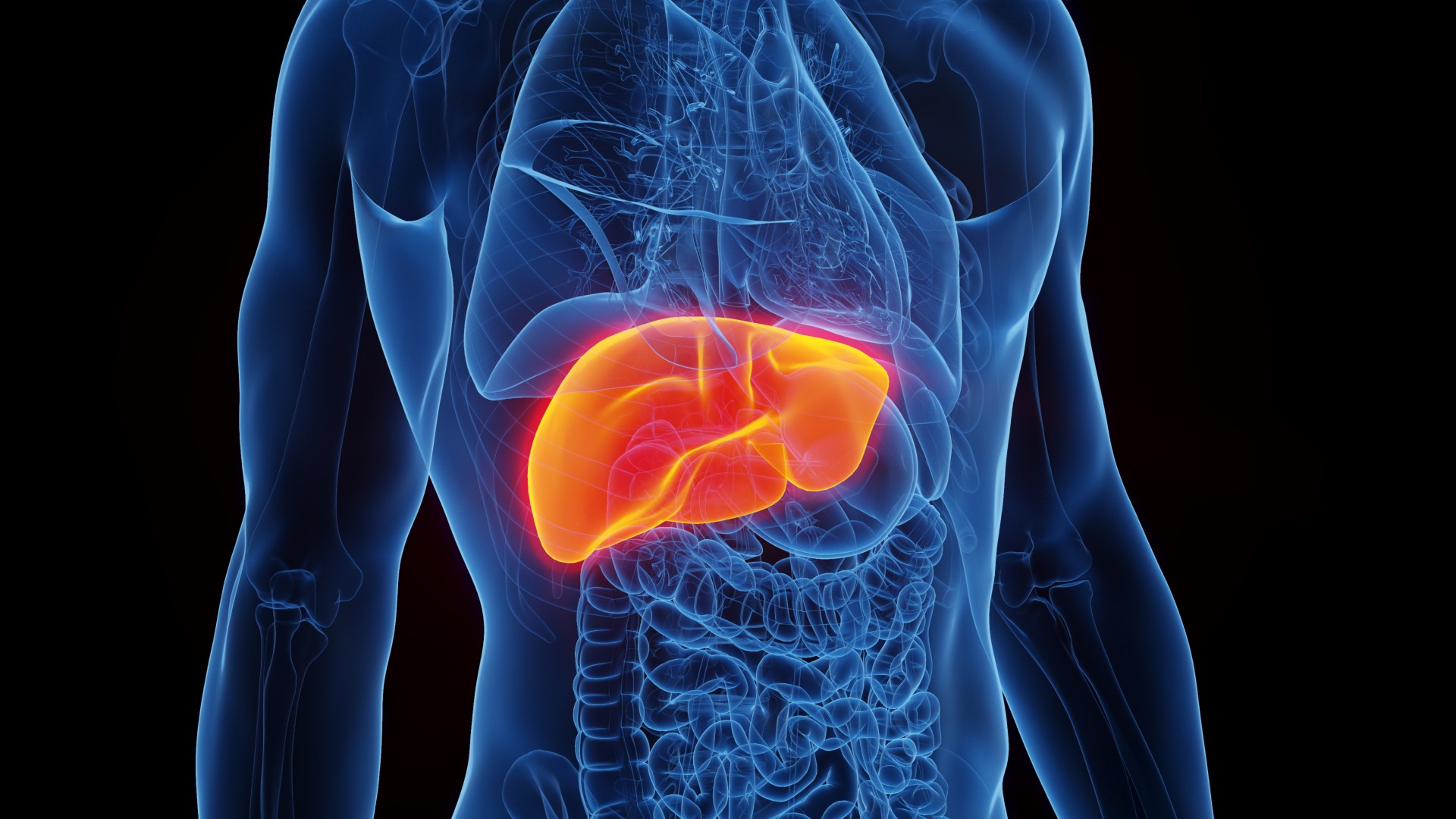
Patients with PFIC develop liver failure as a result of a buildup of a digestive fluid known as bile.
Disease name: Progressive familial intrahepatic cholestasis (PFIC)
Affected populations: PFIC is a group of rare genetic diseases that cause progressive liver failure. The exact prevalence of PFIC is unknown, but estimates suggest that these diseases affect between 1 in 100,000 and 1 in 50,000 people worldwide. In the United States, fewer than 50,000 people total are believed to have PFIC.
Causes: Patients with PFIC have genetic mutations that impair the liver's ability to secrete a digestive fluid known as bile into the digestive tract.
Bile is a yellowish-green fluid produced in the liver, and it is normally secreted into the digestive tract to help with the breakdown of fats, the absorption of vitamins from food, and the removal of waste products in stool.
But in patients with PFIC, bile instead accumulates in the liver and thus begins to damage the organ. As liver cells die, they are replaced with scar tissue, a process known as fibrosis.
Related: Scientists discover new type of cell in the liver
There are three types of PFIC — PFIC1, PFIC2 and PFIC3 — which differ in that they are caused by mutations in different genes that code for proteins needed for the liver to function properly. PFIC is inherited in an autosomal recessive manner, meaning that children must inherit two copies of a relevant mutated gene — one from each parent — to develop the disease.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Symptoms: All patients with PFIC develop symptoms of liver disease, which typically appear during infancy. These symptoms include severe itching; a yellowing of the skin and whites of the eyes, known as jaundice; stunted growth; and high blood pressure in the vein that carries blood from the digestive system to the liver. The itchiness stems from excess bile acid irritating nerve cells in the body.
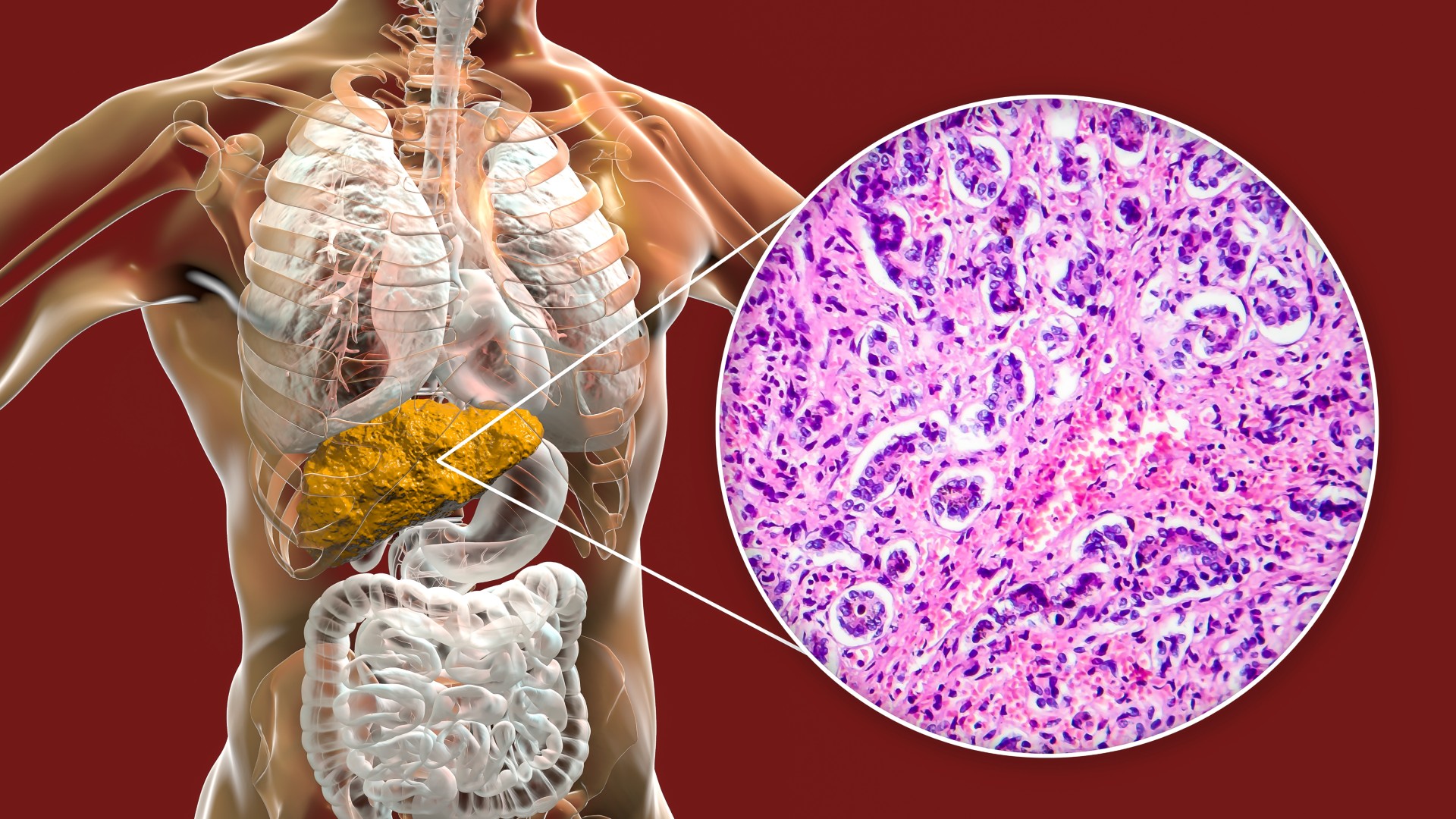
Patients with PFIC1 also may have other symptoms, such as short stature, deafness, diarrhea and inflammation of the pancreas. And those with PFIC2 are at an increased risk of developing a type of liver cancer called hepatocellular carcinoma.
Symptoms of liver failure usually develop before adulthood in patients with PFIC1. The prognosis is typically worse for patients with PFIC2 whose livers fail within the first few years of life. Patients with PFIC3, on the other hand, may develop liver failure in childhood or adulthood.
Treatments: There is no cure for PFIC, but steps can be taken to ease patients' symptoms. For instance, certain drugs can increase the flow of bile out of the liver, while dietary supplements can raise low levels of vitamins and fats in the blood caused by the lack of bile secretion.
Even with these treatments, though, most patients with PFIC will ultimately require a liver transplant. This replaces damaged liver tissue with healthy cells that do not have the genetic defect, thus reversing many symptoms of liver disease.
If left untreated, PFIC kills an estimated 87% of patients. By comparison, several studies have shown that survival rates after liver transplantation range between 76% and 85%; one of these studies followed patients for 19 years after the procedure.
Disclaimer
This article is for informational purposes only and is not meant to offer medical advice.

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.