New trial hints at a possible HIV cure approach: Wake up latent virus hiding in the body, then kill it
A clinical trial of a new method to activate and kill HIV in the body shows small success, but it's not yet a cure.
A new treatment for human immunodeficiency virus (HIV) can drive the virus out of its hiding spots in the body, an early clinical trial finds. That, in turn, raises hopes these reservoirs of HIV could then be wiped out.
The treatment isn't enough to cure HIV on its own. But the new results, published in the Journal of Infectious Diseases on Feb. 13, hint that it could be possible to use this strategy as a step toward curing a person of HIV.
"This is not a home run," said study leader Dr. David Margolis, a professor of medicine, microbiology and immunology, and epidemiology at the University of North Carolina (UNC) Chapel Hill School of Medicine.
"Clearly we need better tools, better drugs, better approaches," he said, "but it does suggest that this strategy itself is deserving of more work."
Related: We could end the AIDS epidemic in less than a decade. Here's how.
HIV in hiding
With modern antiretroviral drugs, doctors can prevent HIV from spreading from cell-to-cell inside the body, allowing people with the infection to live normal lives. Many achieve undetectable viral loads, meaning they cannot transmit HIV to others via sex.
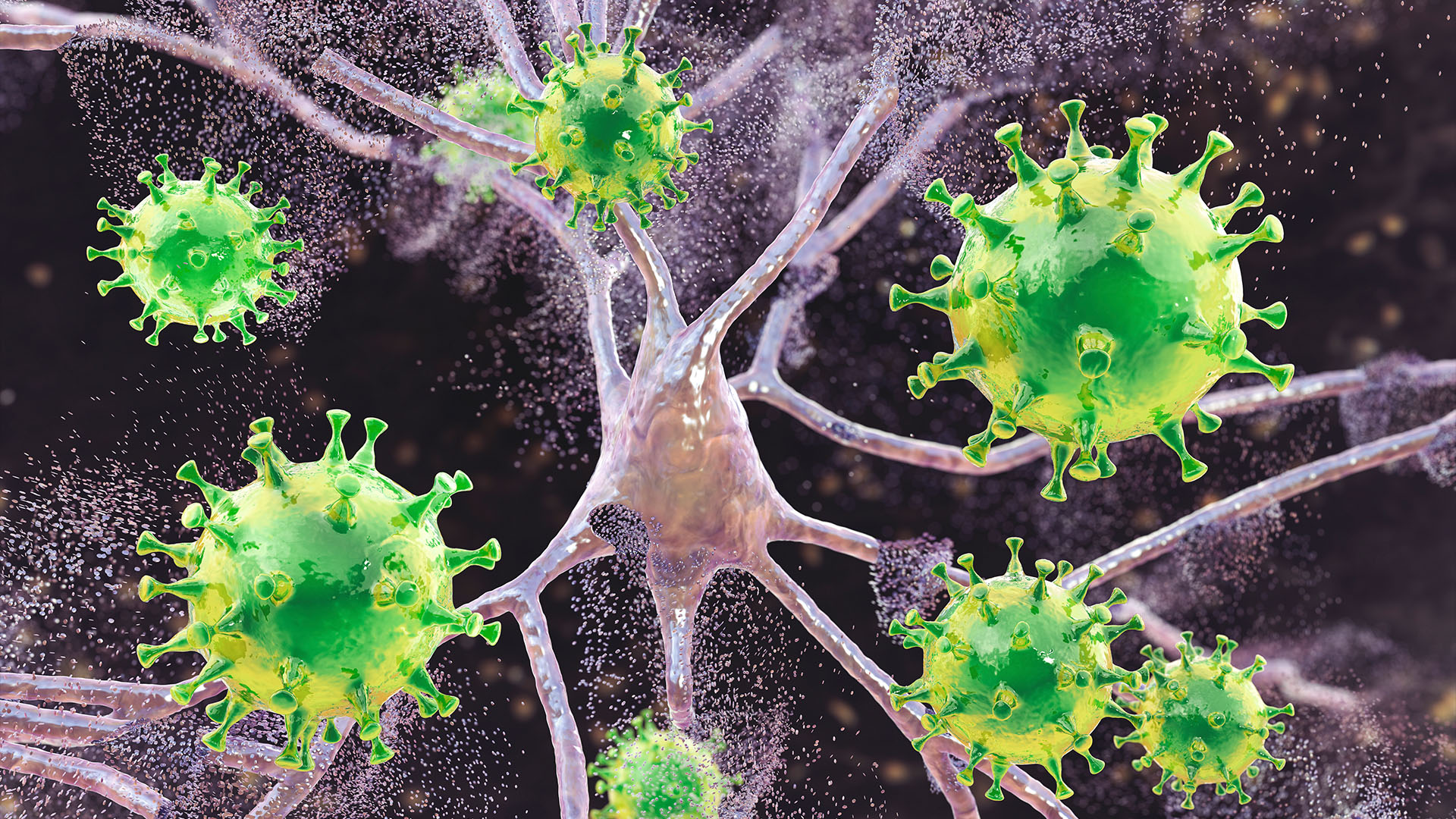
But HIV is a retrovirus, meaning it incorporates its genetic code into cells' DNA and hides out indefinitely, creating a viral reservoir that can retrigger a full-blown infection at any time. To stop an HIV infection from progressing to acquired immunodeficiency syndrome (AIDS), people with HIV must stay on antiretroviral drugs for life.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
To truly cure the infection, the latent HIV reservoir must be driven out and destroyed. That's challenging, though, said Edward Browne, a professor of medicine at UNC's School of Medicine who has previously collaborated with Margolis but was not involved in the recent trial.
HIV hides lots of different types of cells in hard-to-treat places, such as the gut and nervous system. And driving the virus out isn't enough to destroy it.
"We have to hit two home runs at the same time," Browne told Live Science. "We have to reactivate enough viral proteins that the immune system can see it, and we have to get immune effector mechanisms in the right place at the right time to kill them off."
Margolis and his team attempted this with vorinostat, a drug shown to "wake up" HIV from latency in many previous studies. To attack the activated virus, they took patients' own immune cells, identified those programmed to attack HIV, and then grew these cells and reinfused them into the patients.
Six patients in the first phase of the trial got a standard dose of specialized immune cells. Vorinostat did, in fact, reactivate their latent HIV, but the HIV reservoir shrunk in only one patient of the six, by one measurement.
Related: How are people cured of HIV? Here's everything you need to know
In a separate group of three patients, the researchers upped the dose of anti-HIV cells by five times and saw a small decline in the HIV reservoir of all three people. The decline wasn't dramatic enough to take the patients off their HIV-suppressing medications, but it was promising that the results seemed to be dependent on the dose of the immune cells, Margolis said.
"It's a little more convincing that it happened three out of three times with the higher dose and maybe one out of six times at the lower dose," he said.
Reversing latency
Margolis and his team are now working on a strategy using vorinostat and an lab-made antibody against HIV that might do a better job of marking the reactivated virus for destruction. They're also studying another method of reversing HIV latency that seems to work better than vorinostat, which they first described in a 2020 Nature paper.
Several other groups are trying to drive out and kill latent HIV. Some are using medications, others are using immune proteins, while still others are attempting to slice HIV from cells with the gene-editing system CRISPR. Meanwhile, researchers are still unraveling the basic science of HIV latency. Some are exploring the notion of pushing the virus deeper into latency, ensuring that it will never reactivate.
When HIV first emerged, doctors could do little to prevent patients from developing AIDS and dying of related complications, Margolis said. The advent of the first antiretroviral drug changed that. If researchers uncover a working strategy, the landscape of HIV could similarly shift overnight.
"We don't know if we're 20 years away from something that really works or maybe we're just a couple years away from something that works," Margolis said. "There's no way to know."
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Stephanie Pappas is a contributing writer for Live Science, covering topics ranging from geoscience to archaeology to the human brain and behavior. She was previously a senior writer for Live Science but is now a freelancer based in Denver, Colorado, and regularly contributes to Scientific American and The Monitor, the monthly magazine of the American Psychological Association. Stephanie received a bachelor's degree in psychology from the University of South Carolina and a graduate certificate in science communication from the University of California, Santa Cruz.










