'If you don't have inflammation, then you'll die': How scientists are reprogramming the body's natural superpower
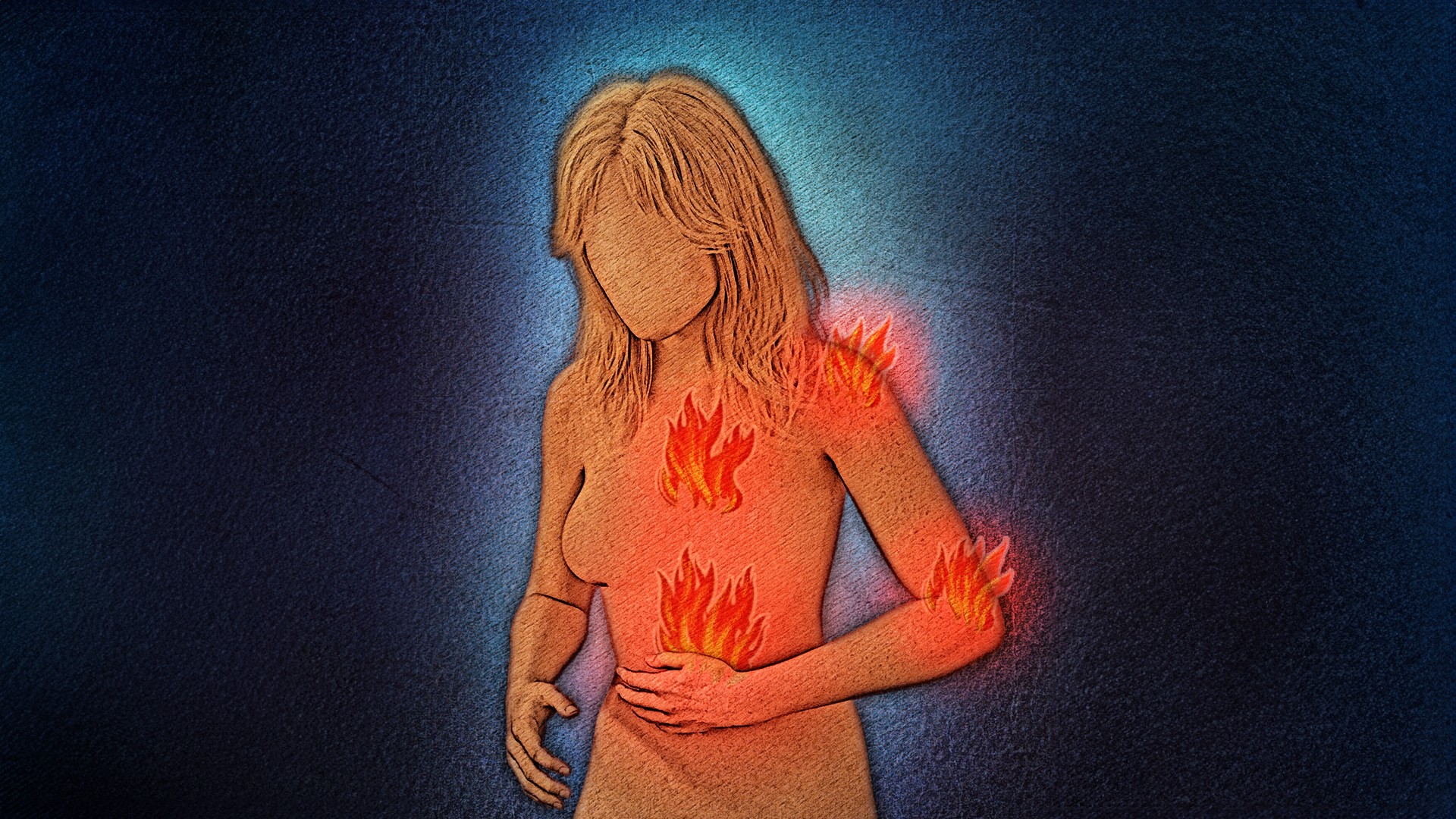
Inflammation can be both a superhero and a villain, depending on the context. Rather than eliminating it completely, new treatments are trying to redirect it.
Inflammation is one of the body's superpowers. It helps us fight off infections and heal wounds.
"If you don't have inflammation, then you'll die," Ed Rainger, a professor who studies chronic inflammation at the University of Birmingham in the U.K., told Live Science. "It's as simple as that."
But if it transitions from a short-term response to one that lingers for months or years, chronic inflammation can fuel diseases such as cirrhosis, rheumatoid arthritis (RA) and heart disease.
In the past, doctors tried to treat these diseases by shutting down all inflammation, which has nasty side effects and doesn't always work. But now, scientists are designing treatments that don't eliminate inflammation altogether but rather reprogram the cells that fuel it.
And in diseases like cancer, where tumors hijack the healing side of inflammation to fuel their growth, new treatments are instead taking the opposite approach — pushing inflammation back into a fighting state so that it can better attack these mutated cells.
Depending on the context, inflammation can be seen as helpful or harmful, but thanks to new research, in either case, it can be brought back under control.
"If you can do that, then you can let the immune system and the inflammatory response get on with it, just in a normal way," Rainger said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Acute and chronic inflammation
Inflammation is the body's natural response to physical trauma, infection or toxins, and doctors have been describing it since antiquity. "Inflammare" means "to set on fire" in Latin, and in the second century, Galen, the physician of Roman emperor Marcus Aurelius, described its five "cardinal signs" as heat, redness, swelling, pain and loss of function.
What these early doctors were describing were the hallmarks of acute inflammation. The redness and heat are caused by the local dilation of blood vessels to ferry more cells to the damaged tissue, while the release of compounds such as prostaglandins cause pain and swelling. To thwart infections, the immune system also cranks out chemicals called pyrogens that further crank up prostaglandin production, causing fever.
"The whole point of inflammation is to control an infection, stop it spreading and then allow the healing process to start," Robert Anthony, an associate professor of medicine at Harvard University, told Live Science.
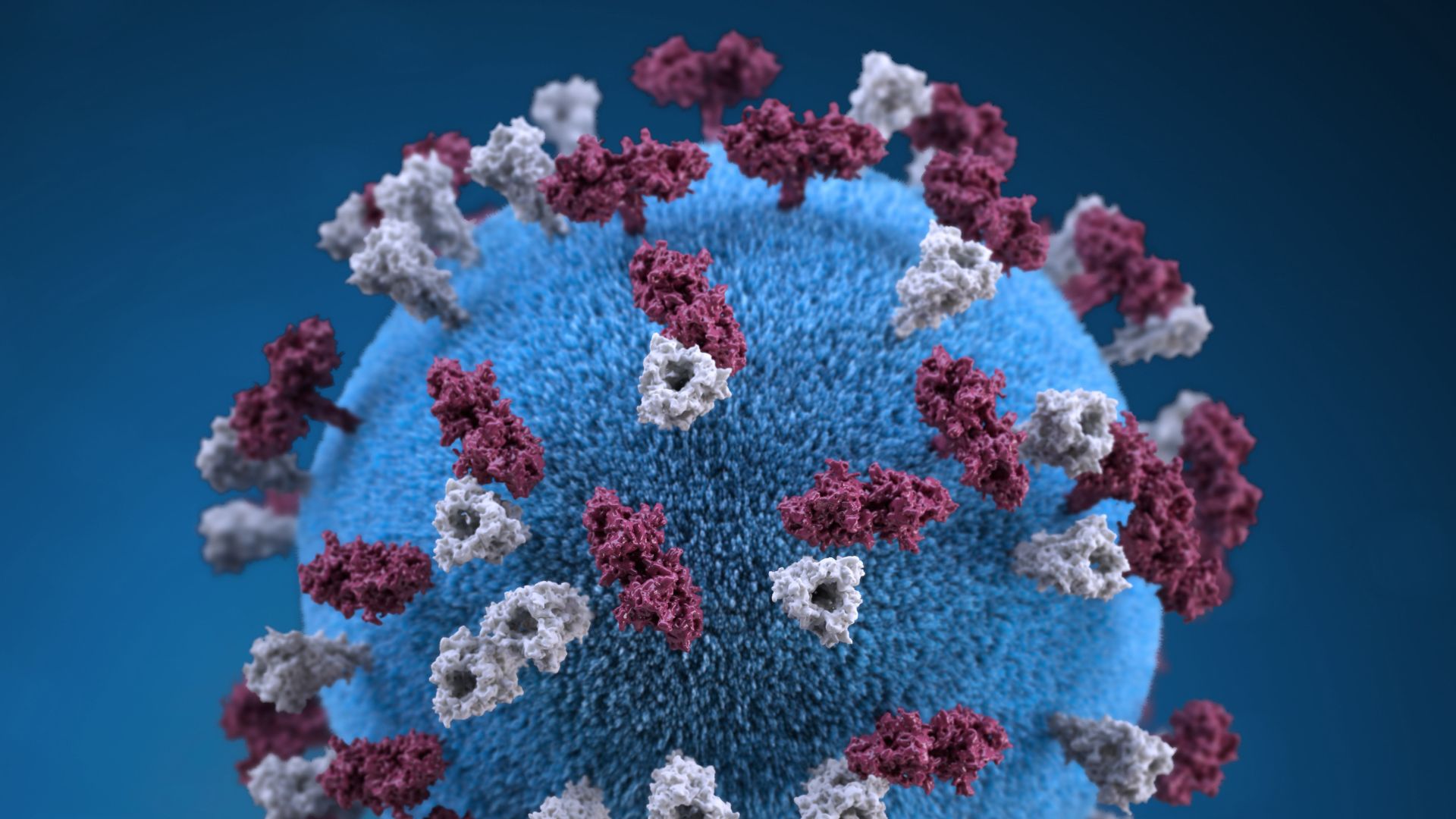
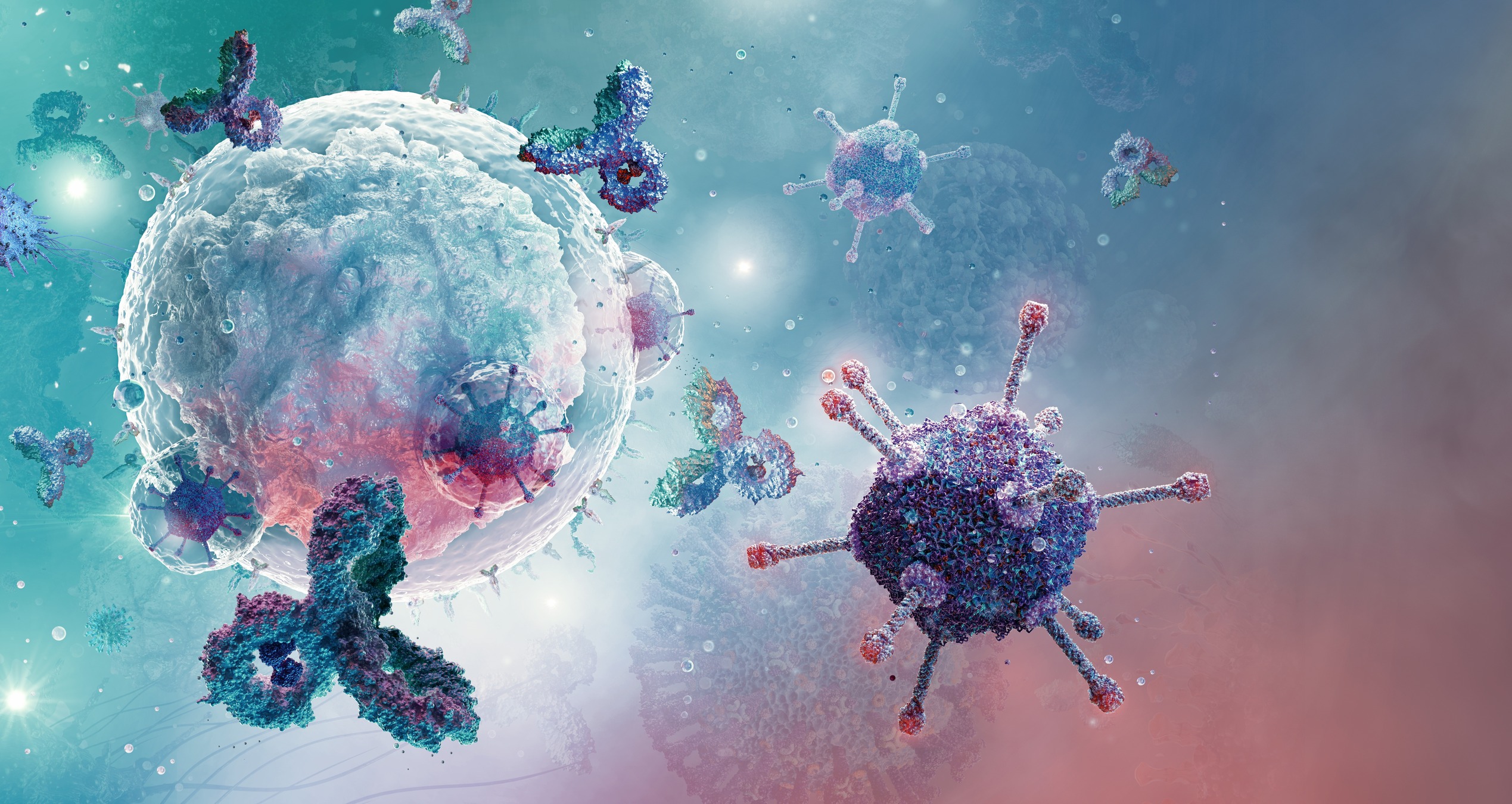
During acute inflammation, damaged cells send out "danger" signals that lure immune cells to the site of the attack. These first responders include the amoeba-like macrophages that gobble up harmful invaders and neutrophils, which trap and kill these enemies. Once activated, these cells produce chemicals called cytokines, which amplify inflammation in a positive feedback loop.
As this acute inflammation rages, the immune system is learning to target the enemy more selectively.
Normally, acute inflammation peaks around seven days after the initial attack and starts to resolve around three days later, Anthony said. At the same time, certain cells work to heal wounds, secreting anti-inflammatory signals and promoting the formation of new blood vessels and connective tissue.
The whole point of inflammation is to control an infection, stop it spreading and then allow the healing process to start
Robert Anthony, Harvard University
Scientists don't fully understand how the body switches off acute inflammation. But sometimes — for instance, if the immune system can't fully control an infection — it doesn't. Then, inflammation can morph from essential to harmful.
If "you stop that transition about day 10, that's when things transition into the chronic phase," Anthony said.
In chronic inflammation, neutrophils, macrophages and other white blood cells linger at the site of inflammation. They churn out cytokines, which keep inflammation amped up. Inflammatory cells also produce growth factors that fuel cell division and enzymes that cause tissue damage, which then sends out more "danger" signals to keep the loop going.
Chronic inflammation is implicated in a range of diseases, including RA, which affects the joints; cirrhosis, or severe liver scarring; and atherosclerosis, or plaques in blood vessels that can lead to heart attack and stroke. And the cellular proliferation and mutation induced by chronic inflammation can create a perfect environment for cancer to develop.
Related: Brain inflammation may drive mood changes in Alzheimer's
Historical treatment
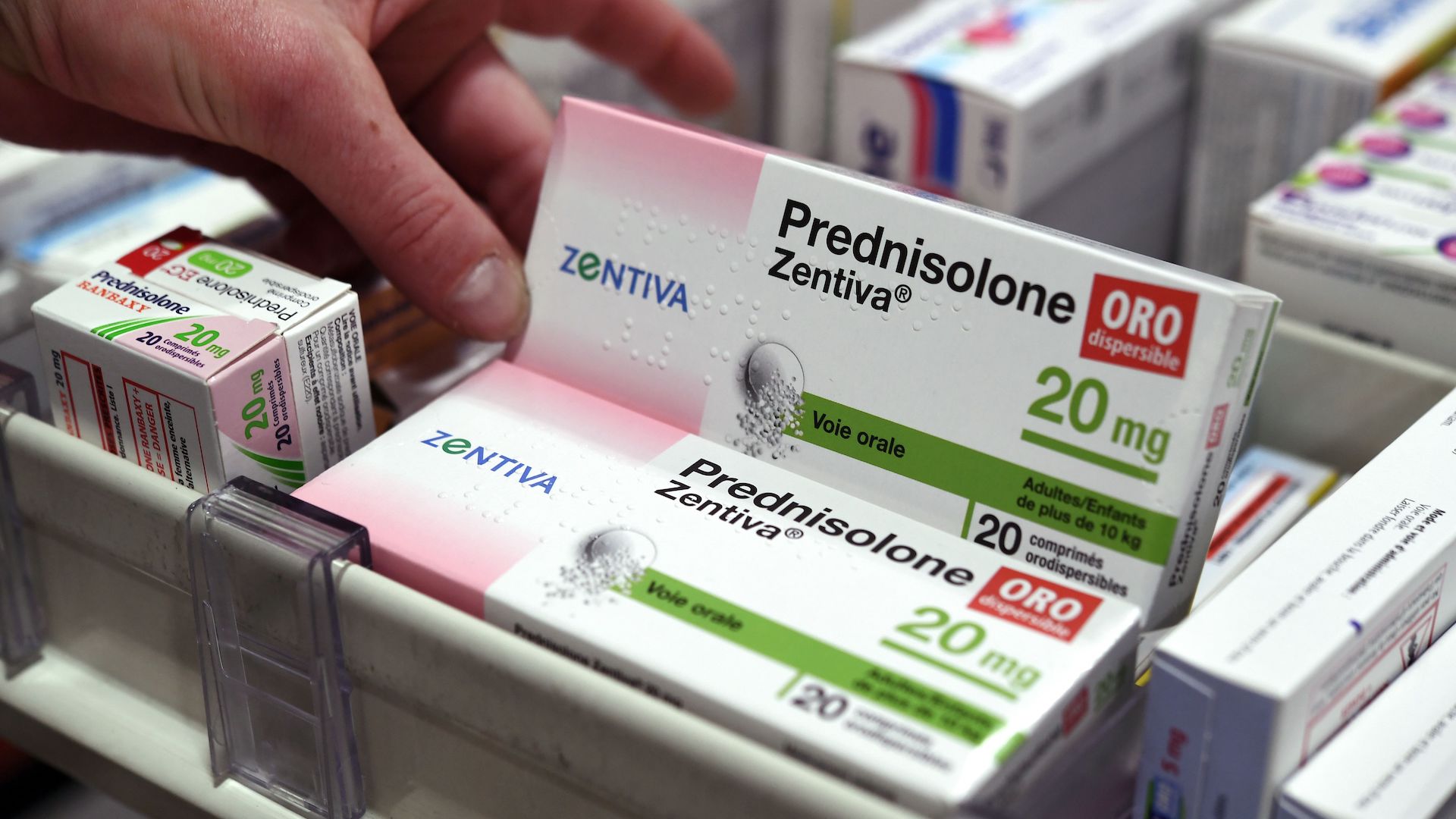
In the past, treatments aimed to silence inflammation altogether. For instance, in the 1950s, scientists discovered the anti-inflammatory effects of a group of naturally occurring compounds called steroids, which turn down the volume on the broader immune response. Since then, steroids have become a mainstay treatment in chronic inflammatory diseases such as RA. But in addition to broadly suppressing the immune system, steroids can cause side effects such as high blood pressure, stomach ulcers and mood swings.
Then, in the 1990s, pharmaceutical companies began rolling out drugs called biologics. Many of these work by silencing different cytokines, the chemical signals that amplify inflammation.
However, like steroids, biologics often suppress large swaths of the immune system, which can increase the risk of infection. For instance, the drug tofacitinib, for RA, targets a signaling pathway which is shared by many cytokines and as a result can make people more vulnerable to herpes zoster virus, pneumonia and urinary tract infections. And for reasons we don't fully understand, biologics don't work for every patient.
So scientists are searching for more targeted ways to redirect harmful inflammation, often by reprogramming immune cells involved in the process.
Related: Why do coughs linger after a cold?
Cellular reprogramming
Stuart Forbes, director of the Centre for Regenerative Medicine and the Institute for Regeneration and Repair at the University of Edinburgh in the U.K., has been studying the role of macrophages in scar tissue formation in liver fibrosis. He and others have found there are actually two types of macrophages: a damaging inflammatory type, dubbed M1, and a second type, called M2. His research in mice found that this second type turned off inflammation and fueled tissue regeneration.
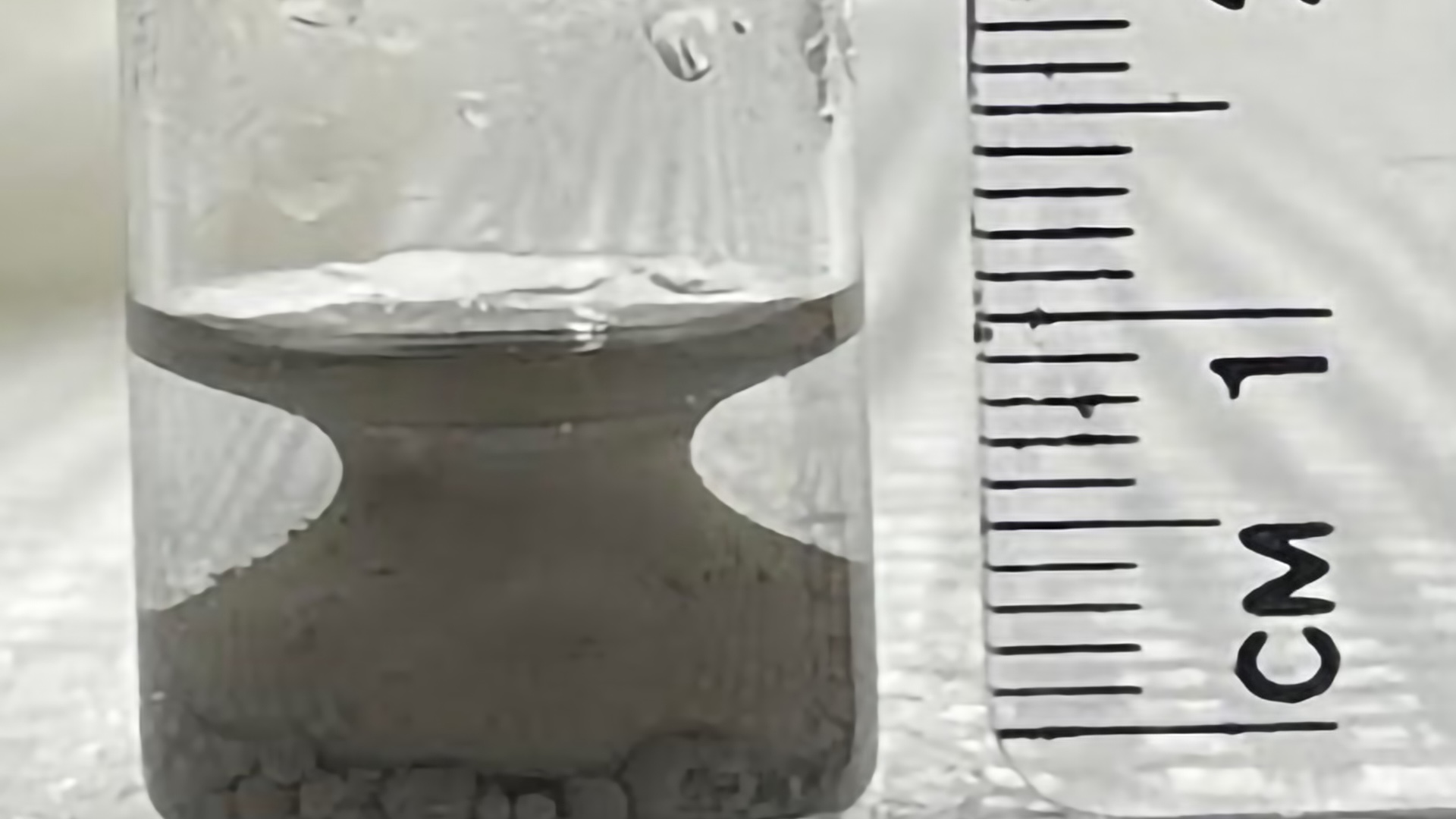
So Forbes' team filters macrophage precursor cells called monocytes from the blood of patients with severe liver scarring. In a lab dish, the team uses chemical signals to nudge these monocytes to become the regenerative, M2 version. Researchers then infuse these reprogrammed macrophages back into patients.
"Using our approach, what we're trying to do is stimulate regeneration of these livers, which means breaking down scar tissue and it means changing the inflammation from damage-forming inflammation to repair-forming inflammation," Forbes told Live Science.
The approach was found to be safe in a Phase I clinical trial of nine patients in 2019, with "encouraging" results from a Phase II efficacy trial in 50 patients presented by Forbes in November at a meeting of the American Association for the Study of Liver Diseases, he said. The team found that over the year-long trial, macrophage treatment decreased the number of potentially fatal, liver-related complications, compared with a control group that did not receive the treatment.
Related: Teen's year-long case of depression and seizures caused by brain-injuring autoimmune disease
Tissue-specific cells
However, to treat the root problem in inflammatory diseases, you need to know the critical cells in specific tissue, Dr. Chris Buckley, a professor of translational rheumatology at the University of Oxford, told Live Science.
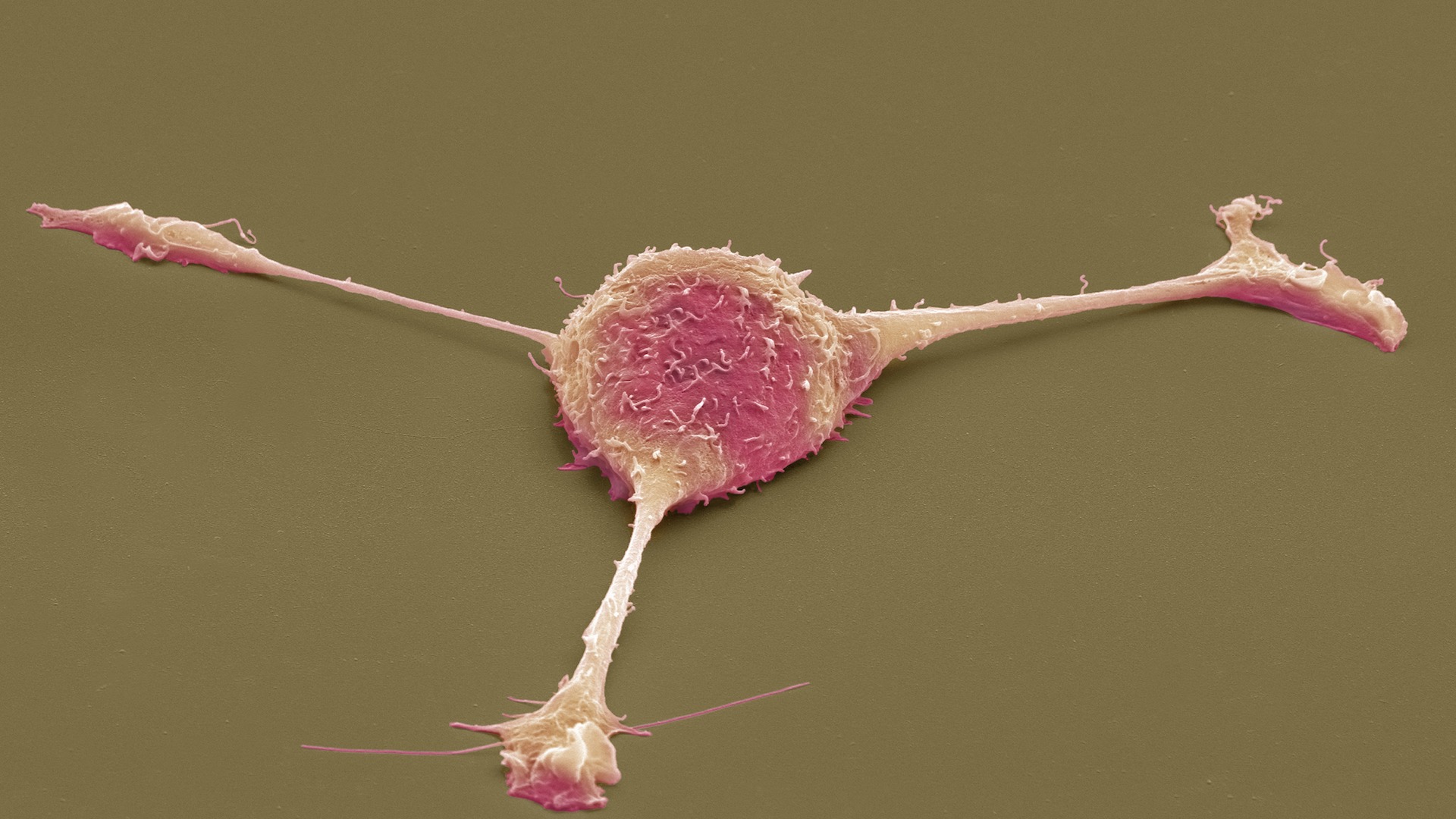
For instance, in RA, white blood cells that are part of the adaptive immune system mistakenly target joint tissue. These white blood cells activate macrophages and connective-tissue-forming cells called fibroblasts, which fuel joint inflammation. Typical RA treatments target the rogue white blood cells. Yet only 50% of patients with RA enter remission.
But in a 2019 paper in the journal Nature, Buckley and colleagues discovered that one type of fibroblast in the joint drives inflammation in RA, while another drives bone and cartilage damage in osteoarthritis. This raises the prospect of treating these diseases by targeting the fibroblasts unique to each condition: inflammatory fibroblasts in RA, and the bone- and cartilage-damaging ones in osteoarthritis.
For RA, for example, if they could target both the white blood cells and the fibroblasts, they might get 100% remission, Buckley said.
The treatment is in its early phases. However, in 2021, a drug called seliciclib, which suppresses the proliferation of fibroblasts in the joints, was found to be safe in a Phase I clinical trial in 15 patients with RA, clearing the path for future trials to assess the drug's efficacy.
Related: DNA-damaging gut bacteria may fuel colon cancer in patients with inflammatory bowel disease
Fanning the flames for good
In some chronic diseases, scientists are developing therapies that stimulate inflammation.
In cancer, for example, macrophages migrate to tumors and attack them, but cancer cells hijack this process, releasing chemicals that cause macrophages to switch from the pro-inflammatory M1 type, to the regenerative M2 type, which suppress inflammation and promotes tumor growth.
Armed with this knowledge, Dr. Yara Abdou, an assistant professor of oncology at the University of North Carolina and her colleagues wondered whether they could use a virus to make macrophages in cancer patients more likely to recognize and attack tumor cells, essentially acting like M1 macrophages.
In 2022, early results from an ongoing Phase I clinical trial of 18 patients with different types of solid cancer — including breast, ovarian and esophageal cancer — showed that treatment with these re-programmed macrophages, called CT-0508, was safe and had promising results.
"We were also able to see that CT-0508 is capable of inflaming the tumor microenvironment," Abdou told Live Science in an email. These macrophages also recruited and activated other immune cells tasked with destroying cancer, she said.
More data from the trial will be reported in 2024, Abdou said. Based on these "encouraging" results, the team also plans to test an alternative version of this therapy called CT-0525, which uses reprogrammed monocytes instead of macrophages, in a Phase I clinical trial in 2024.
Related: What happens to cancer cells after they're killed by treatments?
Next steps
With a Phase II clinical trial under their belt, Forbes and his colleagues want to test an advanced version of their macrophage therapy in patients who have been hospitalized with cirrhosis.
"Currently liver transplant with lifelong care is the only option for patients with advanced liver cirrhosis," Forbes said. Macrophage therapy could therefore provide "a new therapeutic option for this large and growing patient population."
Currently liver transplant with lifelong care is the only option for patients with advanced liver cirrhosis
Stuart Forbes, University of Edinburgh
At the cellular level, Buckley would like to learn more about what drives fibroblasts to both the inflammatory and cartilage-damaging state, teasing out whether the two forms develop from a common precursor cell and determining what factors may regulate this process.
Knowing more about these fibroblasts, both in health and disease, could "unlock their therapeutic potential in tissue repair," Buckley and his colleagues wrote in a 2021 review article.
As for the cancer therapy that is being developed by Abdou and her team, many questions remain, she said. For instance, the team needs to fine tune the exact dose that would be given to patients and assess which type of cancer it may be more effective against.
They're hopeful though that they'll be able to move on to the next stage of testing, a Phase II clinical trial, and if successful, one day, roll it out in patients.
Ultimately, what Abdou and others are doing is reframing the way that we see inflammation; not solely as a flaw to be fixed, but rather an incredible force that can be controlled and harnessed for good.

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)