Could cannabis treat cancer someday? Here's what the science says so far
For decades, cannabis has been studied for its potential antitumor properties, but whether it can actually treat cancer is still unknown.

Research into the potential medical benefits of cannabis has exploded in recent years, raising one intriguing question: Could cannabis treat cancer?
It may sound far-fetched that weed — the high-inducing plant that propagandists once warned would cause "reefer madness" — could contain ingredients that shrink tumors. However, experts told Live Science that there is some early evidence that some cannabinoids, the active ingredients found in cannabis, do have anticancer effects.
"There's no two ways about it: [Cannabis] has anticancer properties," Wai Liu, a senior research fellow at St George's, University of London, told Live Science. "But the problem is, how do you translate that into the clinic — and that's the difficult question to address."
Here's what we know so far about Mary Jane's cancer-fighting powers.
Related: Runners enjoyed their workouts more after using cannabis, but physically floundered
What are cannabinoids, and can they treat cancer?
The cannabis plant comes in more than 700 varieties, with famous examples including Cannabis sativa and Cannabis indica. Cannabis plants contain substances called cannabinoids, or chemicals that interact with the endocannabinoid system in the brain. Endocannabinoids made by the body help regulate a plethora of biological functions, including eating, learning and pain recognition.
Plant-made cannabinoids, of which more than 100 have been identified by scientists, plug into this same system and affect its activity. These plant-made molecules include tetrahydrocannabinol (THC), which is largely responsible for the characteristic "high" associated with cannabis, and cannabidiol (CBD), which doesn't produce a high but has been studied for its potential medicinal effects.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
These and other cannabinoids can now be made synthetically in the lab, as well. In fact, two drugs that contain synthetic THC — dronabinol and nabilone — are already approved by the U.S. Food and Drug Administration to treat the nausea and vomiting triggered by chemotherapy.
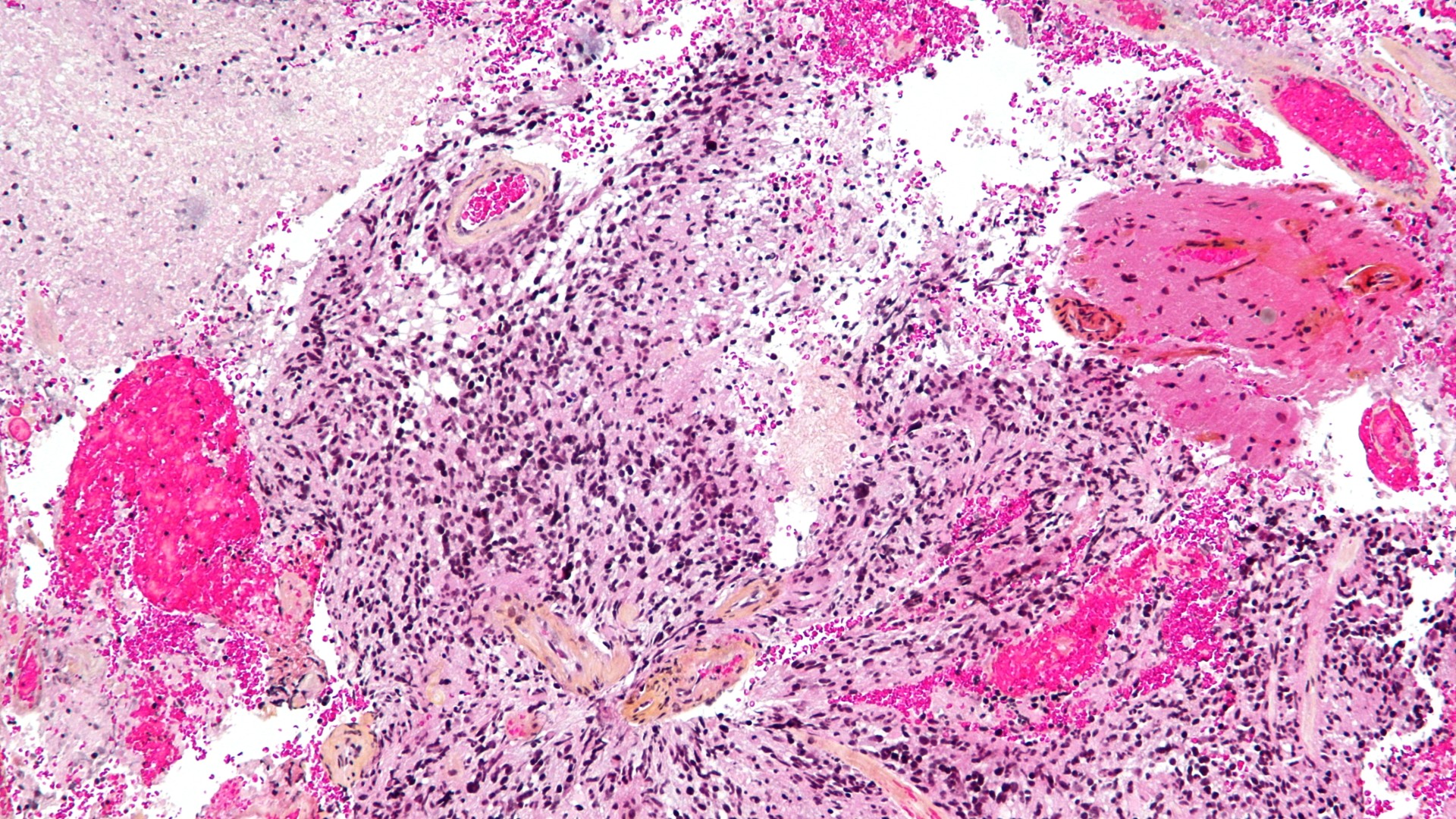
However, research studying whether cannabinoids directly shrink tumors is in its very early days. At this point, it's been mainly limited to preclinical studies in human or mouse cells in lab dishes and in animals such as mice. For instance, synthetic and plant-made cannabinoids have been shown to impede the growth of breast cancer in mice; in these experiments, cannabinoids were injected into the area directly around the tumor, as well as colorectal cancer, prostate cancer and skin cancer in cells.
There are several ways in which cannabinoids have been shown to have anticancer properties, Liu said. For example, in rodent studies, cannabinoids have been shown to inhibit cancer cell growth by flipping specific molecular switches in tumor cells. And in cell studies, cannabinoids have damaged tumors by flooding them with harmful molecules called reactive oxygen species, he said.
However, it's not all positive — under certain circumstances, THC has been shown to promote tumor growth in animal models. These differences could partly be explained by studies using varying doses and investigating distinct types of cancer, the authors suggested.
Related: Cannabis poisonings in young kids skyrocketed following legalization of edibles

Have any cannabinoid-based cancer treatments been tested in humans?
For any cannabinoid-based cancer treatments to reach the market, they'd need to be tested in humans.
"There's a big difference between what you observe in a cell line in a petri dish compared to what will happen if you treat a human who has that cancer," Dr. Mikael Sodergren, head of the Medical Cannabis Research Group at Imperial College London, told Live Science.
However, so far, there have been only a few small clinical trials, and all have focused on just one type of cancer: glioblastoma, the most aggressive form of brain cancer. Current treatments for glioblastoma have poor survival rates meaning that new approaches are urgently needed.
In the first trial, conducted in 2006, scientists showed that THC injections directly into the tumors of patients with brain cancer could safely and effectively inhibit their growth. The trial included just nine patients with glioblastoma. So, although these results were encouraging, the sample size of the study was too small to make any firm conclusions about the drug's safety and efficacy.
In 2021, a separate research group published the results of another early clinical trial, which included 27 people. One group of participants used a mouth spray containing a mixture of CBD and THC in combination with a traditional chemotherapy drug called temozolomide. They received between 3-12 sprays a day (up to 30 milligrams of CBD and 32.4 mg of THC), depending on their maximum tolerated dose. All of the patients had glioblastoma that had returned following standard, first-line therapy.
This trial included a comparison group that did not use the cannabinoid spray, and by comparison, almost twice as many patients who received the spray were alive after one year.
It's still unknown how the spray may affect tumor growth, but it's possible that these compounds help push brain tumor cells toward cell death, thereby enhancing the antitumor activity of temozolomide, Dr. Susan Short, a professor of clinical oncology at the University of Leeds in the U.K. who led the research, told Live Science.
The centres that are running the study are now aiming to recruit around 240 patients into a larger, midstage clinical trial. They hope to be able to share the results of that trial within two years from now, Short said.
What's still unknown?
Despite this progress, many questions remain about how cannabinoids might fight cancer at the molecular level, as well as which dosage and administration route would work best in humans.
And, if approved as a cancer treatment, THC would likely have to be combined with another form of cancer therapy, because only low doses could be given to patients to avoid inducing a high, he said. In clinical trials, it would also be unethical to exclude proven treatment methods from patients, so testing the effects of cannabinoid treatment by itself could be tricky.
In the meantime, the positive signals scientists have seen in cellular models are certainly worth investigating further, Dr. Brooke Worster, an assistant professor of medicine at Thomas Jefferson University in Pennsylvania, told Live Science. Such studies could help clarify how cannabinoids affect cancer cells and which are most promising as treatments.
In the meantime, though, patients should take the results of these studies with a grain of salt, she said. No one should use the early data about cannabinoids to avoid taking treatments that are already known to be effective against cancer, such as immunotherapy and radiation therapy, she said.
There's a misconception that "natural" treatments are always better for you. But given that there isn't gold-standard proof that cannabinoids can treat cancer, opting for weed over chemo wouldn't be advisable, Worster added.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)
Science news this week: Controversy around the dire wolf 'de-extinctions' and a 3D hologram breakthrough
Scientists built largest brain 'connectome' to date by having a lab mouse watch 'The Matrix' and 'Star Wars'
Archaeologists may have discovered the birthplace of Alexander the Great's grandmother