Malaria drug may treat root cause of PCOS, early study hints
A study in humans and lab animals suggests that an antimalarial drug might treat the root cause of PCOS symptoms.

A compound used to treat malaria could potentially alleviate symptoms of polycystic ovary syndrome (PCOS), a small study in humans and lab animals finds.
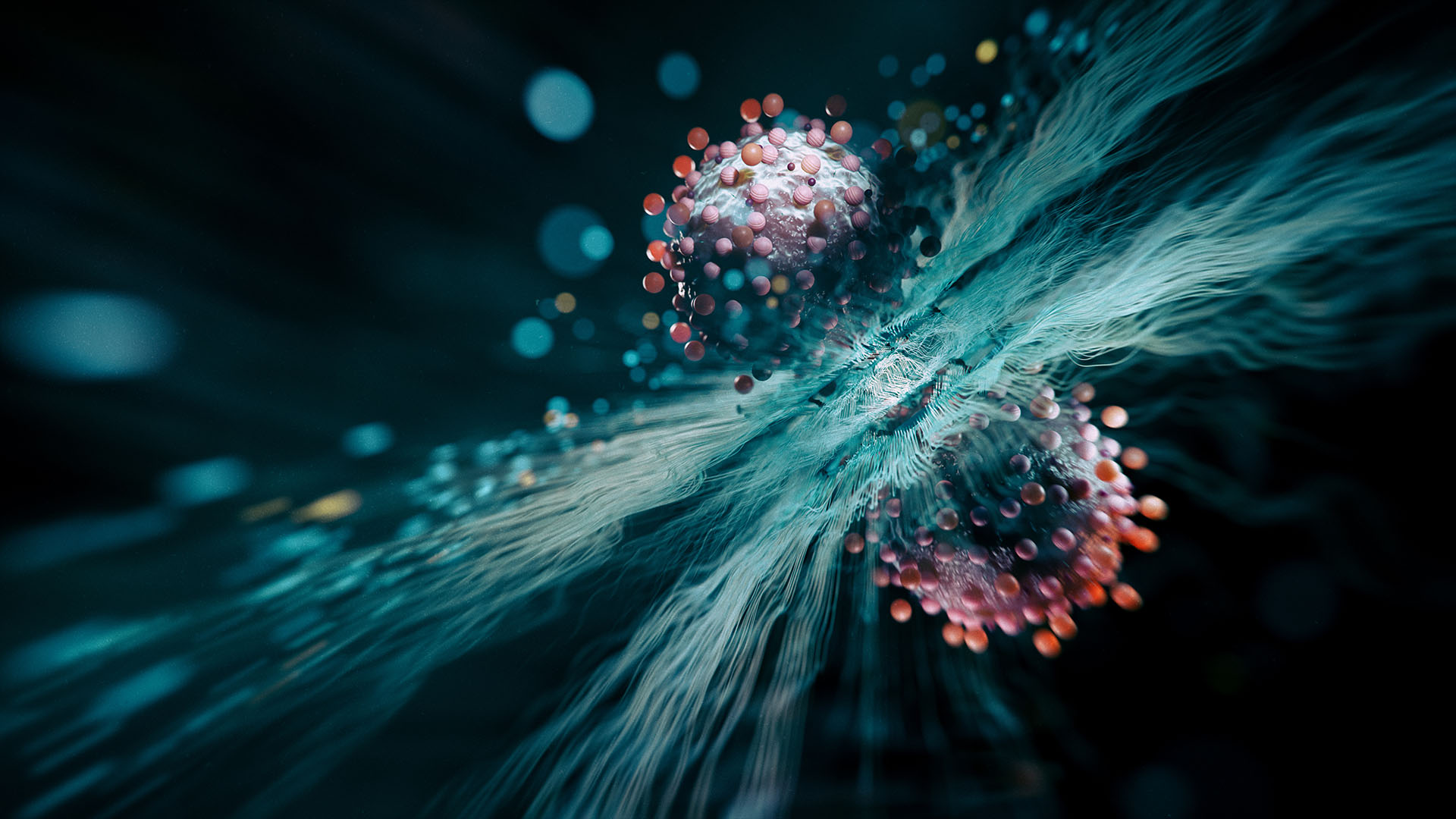
PCOS is a hormonal disorder characterized by high levels of male hormones called androgens. These elevated androgen levels cause a range of symptoms, such as irregular menstrual cycles, excessive hair growth and acne. Complications of the condition include infertility and metabolic problems, including insulin resistance, which raises the risk of type 2 diabetes.
Although PCOS affects 10% to 13% of reproductive-age women, researchers don't completely understand the condition's root cause. It remains difficult to diagnose and treat, and the available treatments — such as birth control pills and blood-sugar-controlling drugs — address only symptoms of the condition.
Now, a new study has shown that an antimalarial drug called artemisinin may ease some symptoms of PCOS, potentially by addressing its root cause.
Related: What does the endocrine system do?
The results, published June 14 in the journal Science, show that artemisinin and its derivatives significantly improved PCOS symptoms, such as irregular hormonal cycles, in both humans and rodents.
For the study, the research team enrolled 19 human participants with symptoms of PCOS, including irregular periods and excess levels of testosterone. Ultrasound also revealed that they had enlarged ovaries with multiple fluid-filled sacs on them; these "follicle cysts" are seen in some, but not all, people with PCOS.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The participants took a derivative of artemisinin by mouth three times a day for three months. There was no group that got a placebo drug, for comparison, so that's one limitation of the study.
The treatment, which had no reported side effects, appeared to lower the testosterone levels in all the participants. In most participants, levels of anti-Müllerian hormone — which the ovaries make too much of in PCOS — also fell.
These hormone changes coincided with a lower number of cysts, less enlargement of the ovaries, and more-regular menstrual cycles in most participants.
The findings suggest that artemisinin is a potential effective treatment for PCOS, said Anna Benrick, a physiologist at the University of Gothenburg in Sweden who was not involved in the research.
However, the study was limited in that it included only a small group of people, and for now, it's unclear whether artemisinin relieves additional PCOS symptoms, such as the metabolic issues, Benrick told Live Science in an email.
To tease out how artemisinin might treat PCOS, the researchers looked to rodents. They found that, in the ovaries of mice and rats, the drug breaks down an enzyme called CYP11A1, which is key for making androgens. This likely prevents the excess production of androgens that drives most PCOS symptoms.
"Because elevated testosterone is one of the main features and cause of most PCOS-related symptoms and comorbidities, treatment aimed at reducing androgen production is a rational target," Benrick said. Artemisinin "represents a promising new approach to lowering those androgens," she said.
However, the animal models were not optimal for studying the metabolic dysfunction seen in PCOS, she added. Studying that in different animal models could give a more complete picture of how well the drug treats the condition.
Future studies could also look at how treating mouse moms with artemisinin affects their offspring, since daughters of mothers with PCOS have a heightened risk of the condition, Benrick said. This is likely due to androgen exposure in the womb, so it would be interesting to see if, by lowering androgens, artemisinin could help prevent PCOS in future generations.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Sneha Khedkar is a biologist-turned-freelance-science-journalist from India. She holds a master's degree in biochemistry and a bachelor's degree in microbiology and biochemistry. After her master's, she worked as a research fellow for four years, studying stem cell biology. Her articles have been published in Scientific American, Knowable Magazine, and Undark, as well as several Indian platforms such as The Hindu and The Wire Science, among others. Besides writing, she enjoys a good cup of tea, reading novels and practicing yoga.