New algorithm dramatically cuts unnecessary antibiotic use in kids
An algorithm reduced rates of antibiotics use in kids treated at Tanzanian primary care facilities without compromising their chances of getting better.

A new algorithm helped doctors in Tanzania cut back on kids' antibiotics prescriptions by more than 46% without compromising the children's chances of recovery, a new study reveals.
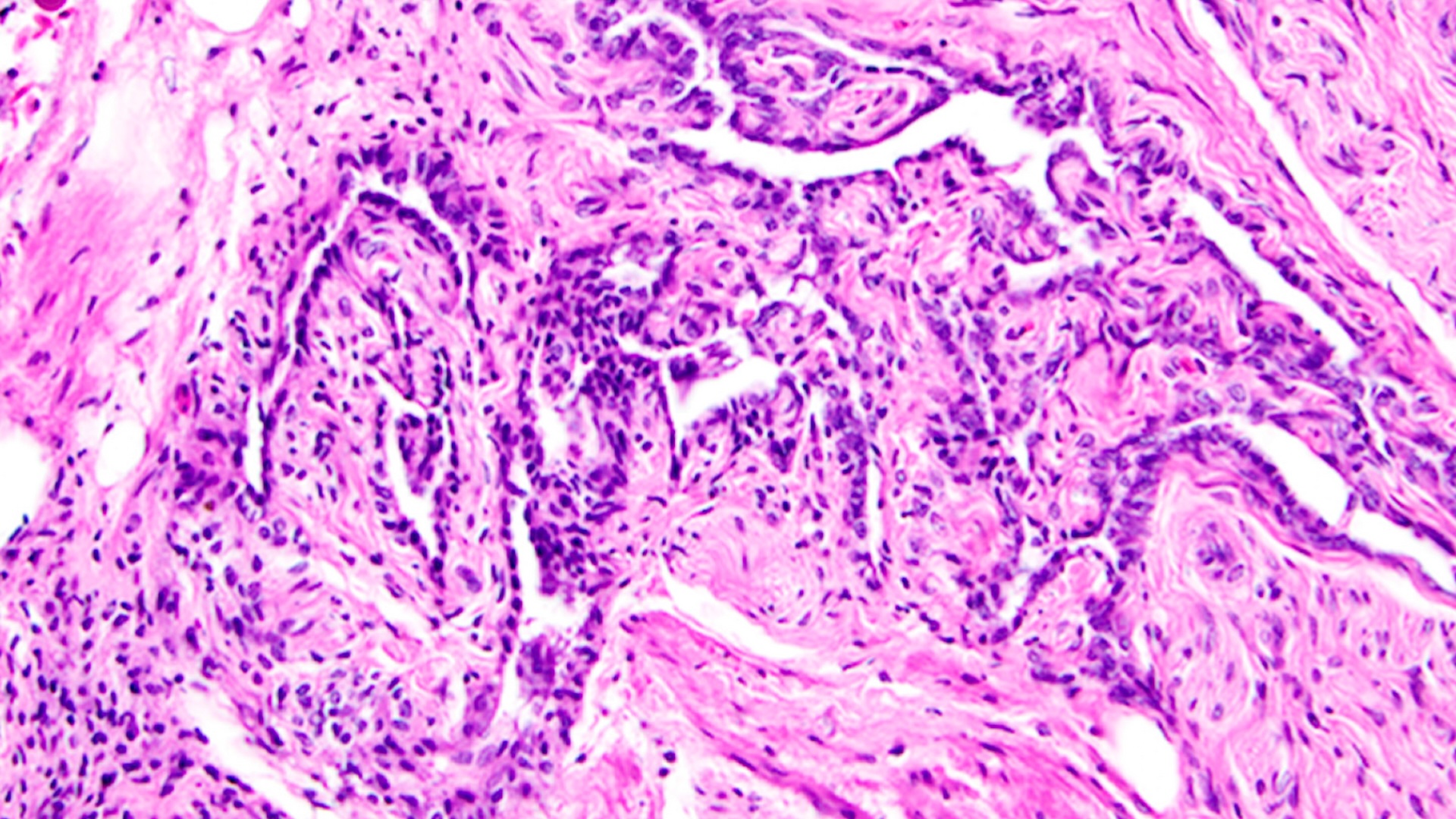
Antibiotic overuse is a major driver of drug resistance worldwide, as it pressures bacteria to evolve new strategies to survive and grow even when exposed to antibiotics. This makes bacterial infections progressively harder to treat as existing antibiotics become less effective.
Past studies suggest that, at U.S. outpatient health care facilities, at least 28% of antibiotics prescribed are not actually needed. In Tanzania, more than 50% of sick children receive antibiotics when visiting health care facilities, and most often, these are not appropriate for the given child's illness, the authors of the new study wrote.
Now, a new algorithm, described in a report published Monday (Dec. 18) in the journal Nature Medicine, has shown promise in guiding doctors to prescribe antibiotics appropriately, only when needed.
Related: Superbugs are on the rise. How can we prevent antibiotics from becoming obsolete?
The new algorithm, called ePOCT+, is a digital tool that guides health care providers through what signs and symptoms to look for in a patient; which tests to run; what the likely diagnosis is; and what the best course of treatment would be. In short, it flags when it makes sense to prescribe antibiotics and when it would not.
The algorithm can incorporate data from several quick-turnaround tests that can be conducted during a doctor's appointment, known as point-of-care tests. These include, for instance, tests for oxygen levels in the blood, the levels of oxygen-carrying protein hemoglobin in blood, and inflammation levels. These quick measures can provide hints as to whether a child has a bacterial or viral infection, whereas testing for the bacteria itself would take hours.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The trial included 40 healthcare facilities across Tanzania that were randomly split into two groups: one that used the algorithm and one that didn't.
Over the course of 11 months, the researchers monitored antibiotics prescriptions at both sets of facilities. They zoomed in on consultations for about 44,300 kids younger than age 15, ranging from infants to young teens. Most of these consultations were the patient's first visits to the doctor about a problem, while a minority were patients returning to the facility about an ongoing issue.
At health care facilities that used ePOCT+, about 23% of kid's initial consultations resulted in an antibiotics prescription, compared with more than 70% at the usual-care facilities. The return visits included in the study saw a similar-size drop in antibiotics prescriptions at facilities that used the algorithm.
Following the algorithm "resulted in a close-to three-fold reduction in the likelihood of a sick child receiving an antibiotic prescription compared to children in usual care facilities," the authors wrote in the study.
However, despite this big difference, a week out from those doctors' visits patients in both groups were doing about the same. There wasn't a significant difference in the percentage of patients who grew subjectively worse, needed hospitalization or died between the two groups. However, significantly fewer children treated at the ePOCT+ facilities had to return for a second consultation after their first.
These results suggest algorithms like ePOCT+ could help cut down on antibiotics use without harming patients, the authors concluded. However, it's important to note that, while most health care providers at the ePOCT+ facilities used the algorithm, not all did — the tool wasn't used in nearly 25% of the consultations reviewed in that arm of the study.
If the tool was used more consistently, they may have seen even better results, the authors wrote. "Widespread implementation of ePOCT+ could help address the urgent problem of antimicrobial resistance by reducing excessive antibiotic prescription in sick children while maintaining clinical safety," they concluded.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.