New mRNA therapy shows promise in treating 'ultrarare' inherited disease
Initial trial results suggest that a new mRNA therapy may be able to safely and effectively treat propionic acidemia, a rare metabolic disorder.
A new treatment may be able to treat a life-threatening disorder that predominantly affects children, initial findings from a pioneering clinical trial suggest.
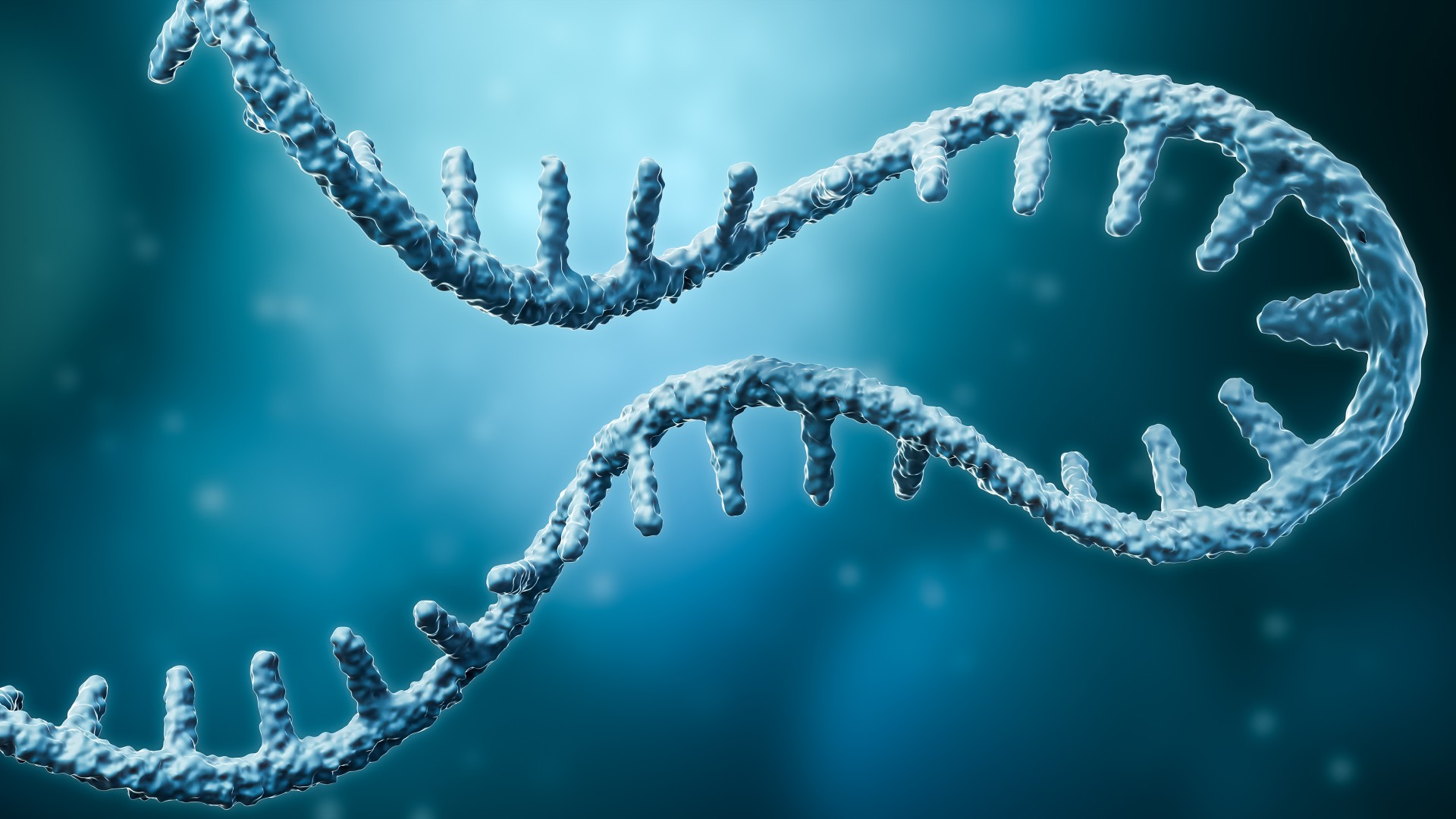
The disorder, called propionic acidemia (PA), is an inherited metabolic disorder that affects around 1 in 100,000 people in the U.S. Individuals with the disease have faulty copies of genes needed to make parts of the enzyme propionyl-coenzyme A carboxylase (PCC), which breaks down the building blocks of certain proteins and fats.
Without fully functional PCC enzymes, harmful compounds accumulate in the body, triggering recurrent symptoms known as "metabolic decompensation events" (MDE). These episodes include lethargy, vomiting, dehydration, and in serious cases, potentially coma and death. In most instances, symptoms of this rare disorder become apparent a few days after birth.
There is currently no cure for PA. Instead, treatments aim to manage the symptoms of the disease, by getting patients to follow a carefully controlled, low-protein diet, for example, and frequently replacing lost fluids to prevent dehydration. Patients may also require liver transplants, as replacing this key organ involved in metabolism can help somewhat restore their levels of functioning PCC.
But now, scientists are testing a new therapy for PA that uses messenger RNA (mRNA) — a genetic molecule that contains the instructions cells need to make proteins. The same type of molecule serves as the basis of the COVID-19 vaccines made by Pfizer and Moderna. The new treatment, called mRNA-3927, contains mRNA needed to make the two subunits of PCC that are faulty in patients with PA, thus helping to replenish stocks of working enzymes in the body.
Related: New mRNA 'cancer vaccine' trial launches in UK
In the recent trial, described Wednesday (April 3) in the journal Nature, scientists enrolled 16 patients with PA, whose ages ranged from 1 to 28. Twelve participants completed this interim analysis.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The patients were split into five groups, and each group was given injections of varying amounts of mRNA-3927 over a few weeks to see what dose of the treatment worked best with the fewest side effects. After this dose adjustment period, 12 patients continued the treatment in an "open-label" or unblinded study, but the researchers have primarily analyzed data from the first phase of the trial.
Eight of the 16 participants had experienced MDEs in the year before the trial, and these patients saw an overall 70% drop in their rate of MDEs during treatment.
All but one of the 16 patients experienced treatment-induced side effects, such as vomiting, diarrhea and fever. But these effects were not serious enough to warrant reducing or halting the treatment, the researchers reported.
"This research could potentially improve outcomes for patients with propionic acidemia, who are at risk for recurrent illnesses requiring hospitalization, impaired growth and development, and early mortality," Dr. Dwight Koeberl, a professor of pediatrics at Duke University School of Medicine in North Carolina who was not involved in the research, told Live Science in an email.
The trial has several key limitations, including that it only tested mRNA-3927 in a small group of patients, as this was an early safety trial. It also didn't include a comparison group of patients with PA who didn't receive mRNA-3927. Without this direct comparison, the team can't yet definitively say how effective the treatment is.
However, these are only preliminary findings from an ongoing trial. At the time of writing up the Nature study, the researchers noted that two patients had dropped out after the initial dosing phase and another two were still being investigated. The rest were receiving ongoing treatment in the open-label trial, getting injections about two or three times a week.
After determining the optimum dose of mRNA-3927, the team hopes to assess the treatment's longer term safety and effectiveness over the course of a year, to see if these promising findings endure.
"It is very encouraging to see promising results in the first-in-human trial [of this therapy]," and it provides hope for treating other similar diseases, Pawel Swietach, a professor of physiology at the University of Oxford who was not involved in the research, told Live Science in an email.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)
What are mRNA vaccines, and how do they work?
Deadly motor-neuron disease treated in the womb in world 1st