What are mRNA vaccines, and how do they work?
mRNA vaccines train the immune system in a similar way to traditional vaccines, but they use a different strategy to get there.

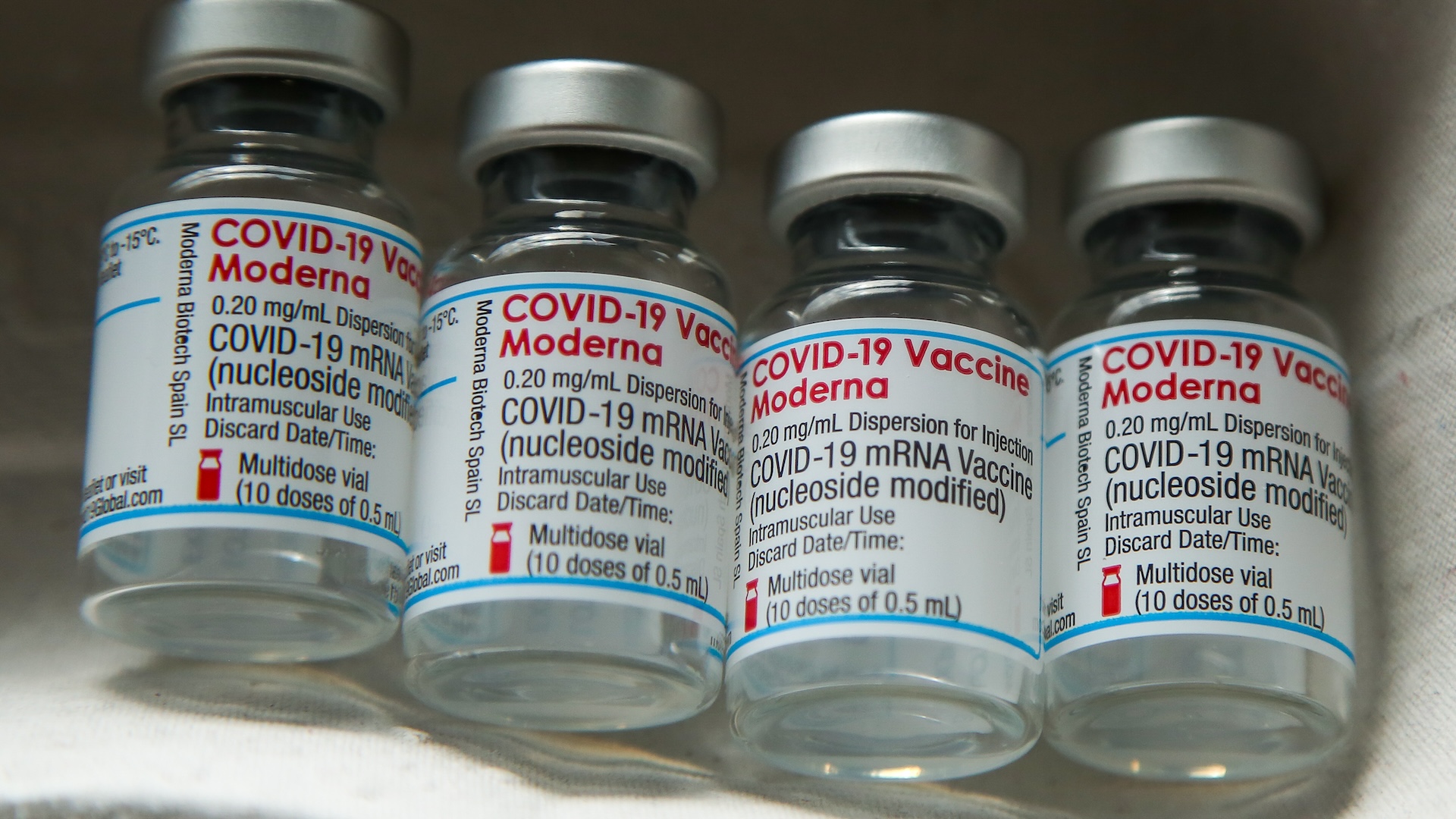
Many people first learned about mRNA vaccines during the coronavirus pandemic, when the companies Pfizer-BioNTech and Moderna released their COVID-19 vaccines. The Pfizer-BioNTech shot was the first COVID-19 vaccine to earn emergency authorization in the United States, and later, it would become the first mRNA vaccine of any kind to be fully approved by the U.S. Food and Drug Administration (FDA).
But even though these firsts took place during the pandemic, mRNA vaccines had been in development for many years before COVID-19 emerged as a threat.
Looking forward, they'll likely continue to play a big role in preventing — and even treating — other diseases in the future.
So what, exactly, are mRNA vaccines, and how do they work?
How do mRNA vaccines work?
mRNA vaccines teach the immune system to target specific proteins, often proteins found on a pathogen, like a virus. To do this, they use instructions carried in a genetic molecule called messenger RNA (mRNA).
Although they're unique in that they use mRNA, these vaccines still employ very similar strategies as traditional vaccines — such as the approved shots for measles, tetanus or the flu — to protect against infectious diseases.
"All vaccines work by teaching your immune system to recognize specific immune signals called antigens," Dr. Vinod Balanchandran, director of the Olayan Center for Cancer Vaccines at Memorial Sloan Kettering Cancer Center, told Live Science in an email. "Antigens are proteins, or even pieces of proteins, that the body recognizes as 'foreign.'"
Traditional vaccines teach the immune system to recognize antigens from viruses or bacteria by directly exposing the body to antigens from that germ. A given vaccine might contain the whole germ, but a version that's been weakened or killed so it can't cause disease. Alternatively, a shot may carry only a piece of the germ that contains the antigen of interest.
When the immune system detects a new antigen, it learns to recognize it as a potentially dangerous invader. After this training, if the immune system sees that antigen again in the context of a real infection, it can quickly recruit the body's defenses and fend off the germ before it takes hold and causes serious illness. The most effective vaccines can prevent even mild cases of infection.
Rather than carrying any antigens, mRNA vaccines contain only the genetic instructions for the antigen of interest. These genetic instructions are encoded in mRNA, a molecule found in all human cells. mRNA often acts as an intermediary molecule, carrying the blueprints for building proteins from the cell's nucleus to a protein-making factory, called a ribosome.
Once an mRNA vaccine is administered, our cellular machinery follows the genetic instructions it contains to produce copies of an antigen. This then enables the immune system to familiarize itself with the antigen, as it would with any other type of vaccine.
What ingredients are in mRNA vaccines?
In addition to the mRNA itself, mRNA vaccines contain a few other ingredients, which vary slightly by the vaccine and manufacturer but fall into a couple of common categories.
These include lipids, or fats, which help form a protective coating around the mRNA that keeps it safe in the body and enables it to easily slip into cells. Different types of sugars, salts, acids and chemical stabilizers also may be included in a given vaccine to help balance the acidity of the formula and keep its temperature stable.
These ingredients help ensure that the vaccine has time to complete its job before the drug is broken down by the body.
How many mRNA vaccines have been approved?
So far, the only mRNA vaccines to be approved by the FDA are the coronavirus vaccines produced by Pfizer-BioNTech and Moderna.
Other mRNA vaccines are in various stages of development, including shots to prevent influenza, Ebola, Zika virus and HIV, as well as shots aimed at treating and preventing cancer.
Were mRNA vaccines made "too quickly"?
To some people, it may seem like mRNA vaccines came out of nowhere, but the technology has actually been in development for over 30 years.
mRNA molecules were discovered in 1961, and by 1978, scientists were experimenting with ways of delivering the molecules into mouse and human cells. Scientists first tested mRNA injections on living mice in 1990, and the first human clinical trials for an mRNA-based rabies vaccine began in 2013.
It took a long time for scientists to figure out an effective way to deliver mRNA molecules into the body without the delicate molecules degrading. So, although the development of the coronavirus mRNA vaccines seemed quick, it was actually preceded by decades of research.
Now that the basic technology for mRNA vaccines exists, a great advantage of the shots over traditional ones is that they can be produced quickly in response to new pathogens. And they can be quickly updated for pathogens that evolve quickly, picking up new mutations and giving rise to new variants.
As an example, the annual flu vaccine is manufactured primarily using viruses cultivated in chicken eggs — a process that takes six months to make all of the needed doses. By comparison, "mRNA vaccines can be developed and manufactured at a faster rate than other kinds of vaccines, which may be important when a new virus emerges or evolves quickly like we have seen with SARS-CoV-2," the virus that causes COVID-19, Melissa Dibble, a former spokesperson for the Centers for Disease Control and Prevention (CDC), told Live Science in an email.
Can mRNA vaccines affect your DNA?
mRNA vaccines do not affect DNA.
"The genetic material delivered by mRNA vaccines never enters the nucleus of your cells, which is where your DNA is kept, so the vaccine does not alter your DNA," Dibble said.
Furthermore, "after the body produces an immune response, it gets rid of all the vaccine ingredients just as it would get rid of any information that cells no longer need," she said.
Typically, an mRNA vaccine takes a few days to be fully broken down by the body.
What are possible side effects of mRNA vaccines?
The COVID-19 mRNA vaccines have been shown to be safe, with most reported side effects being mild and temporary. These side effects, which are also seen in people given traditional vaccines, include pain or swelling at the injection site, headache, fatigue, muscle or joint pain, nausea, chills and fever.
Serious side effects are very rare. For example, anaphylaxis, a severe allergic reaction that can potentially occur after any type of vaccination, occurs in about 5 out of every 1,000,000 COVID-19 mRNA vaccine doses.
Myocarditis and pericarditis — which respectively involve dangerous inflammation in or around the heart — can happen very rarely in response to mRNA vaccines against COVID-19, but these conditions typically respond well to treatment. It's also important to note that both myocarditis and pericarditis are potential complications of a COVID-19 infection itself, and that the risk of developing heart complications from an infection is about ten times greater than the risk from the vaccine.
Based on these data and data from clinical trials, experts have concluded that the benefits of mRNA vaccines far outweigh any potential risks.
What is "frameshifting," and should I be concerned?
A 2023 study published in the journal Nature suggested that the body can sometimes accidentally make a small amount of the wrong proteins based on the genetic instructions from an mRNA vaccine. The study was conducted in lab mice and a group of 20 human participants.
The effect was caused by a knock-on immune response, the researchers reported, and it happened due to a phenomenon called "frameshifting," in which a cell's protein-making machinery starts reading an mRNA molecule at the wrong point of its sequence.
Most of the time, the cell detects that the frameshifted instructions are nonsense, and it stops making the protein. But every now and then, a cell may produce a small quantity of the wrong protein. However, the Nature study found that these frameshifted proteins weren't harmful and that none of the study participants who experienced this response had any vaccine side effects. And notably, cells don't continue to make the frameshifted protein after the mRNA has broken down, so this is a temporary effect.
Frameshifting is not uniquely associated with mRNA vaccines — it also occurs during actual viral infections. Viruses replicate inside the body by hijacking cellular machinery to copy their viral DNA, and frameshifting can often happen during this process, too. In fact, the researchers of the Nature study suggest that exposure to frameshifted proteins might help the body develop broader immunity to a virus.
The authors of the study emphasized that neither the frameshifting or knock-on immune responses they observed compromise the safety of mRNA vaccines. However, they suggested that future mRNA vaccines be designed with molecules that prevent protein-making machinery from "slipping" around the mRNA strand. This would help cells read the mRNA more accurately, without frameshifts, and make new vaccines even more precise.
The future of mRNA vaccines
Although mRNA vaccines rose to prominence during the coronavirus pandemic, their applications stretch far beyond infectious diseases.
Today, many cutting-edge research groups are exploring the potential of mRNA technologies to treat conditions such as Celiac disease, lung damage, preeclampsia, brain cancer and pancreatic cancer.
"We are very excited about the application of mRNA vaccines to treat cancer," Balachandran said. "In our work on cancer vaccines, we use mRNA technology because it is amenable to rapid and flexible production, allowing us to customize a vaccine for every patient." Cancer vaccines generally work like a kind of immunotherapy, priming the immune system to go after tumor cells that can otherwise hide from its attacks.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Editor's note: Live Science spoke to Melissa Dibble prior to recent layoffs at the CDC, which the communications department was impacted by.
Disclaimer
This article is for informational purposes only and is not meant to offer medical advice.

Marilyn Perkins is the content manager at Live Science. She is a science writer and illustrator based in Los Angeles, California. She received her master’s degree in science writing from Johns Hopkins and her bachelor's degree in neuroscience from Pomona College. Her work has been featured in publications including New Scientist, the Johns Hopkins Bloomberg School of Public Health magazine and Penn Today, and she was the recipient of the 2024 National Association of Science Writers Excellence in Institutional Writing Award, short-form category.
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.