'This is largely uncharted territory': Scientists reveal the brain's 'fear circuit' works differently than we thought
New methods applied in live mice suggest that molecules called neuropeptides, not neurotransmitters, play the main role in our response to danger.
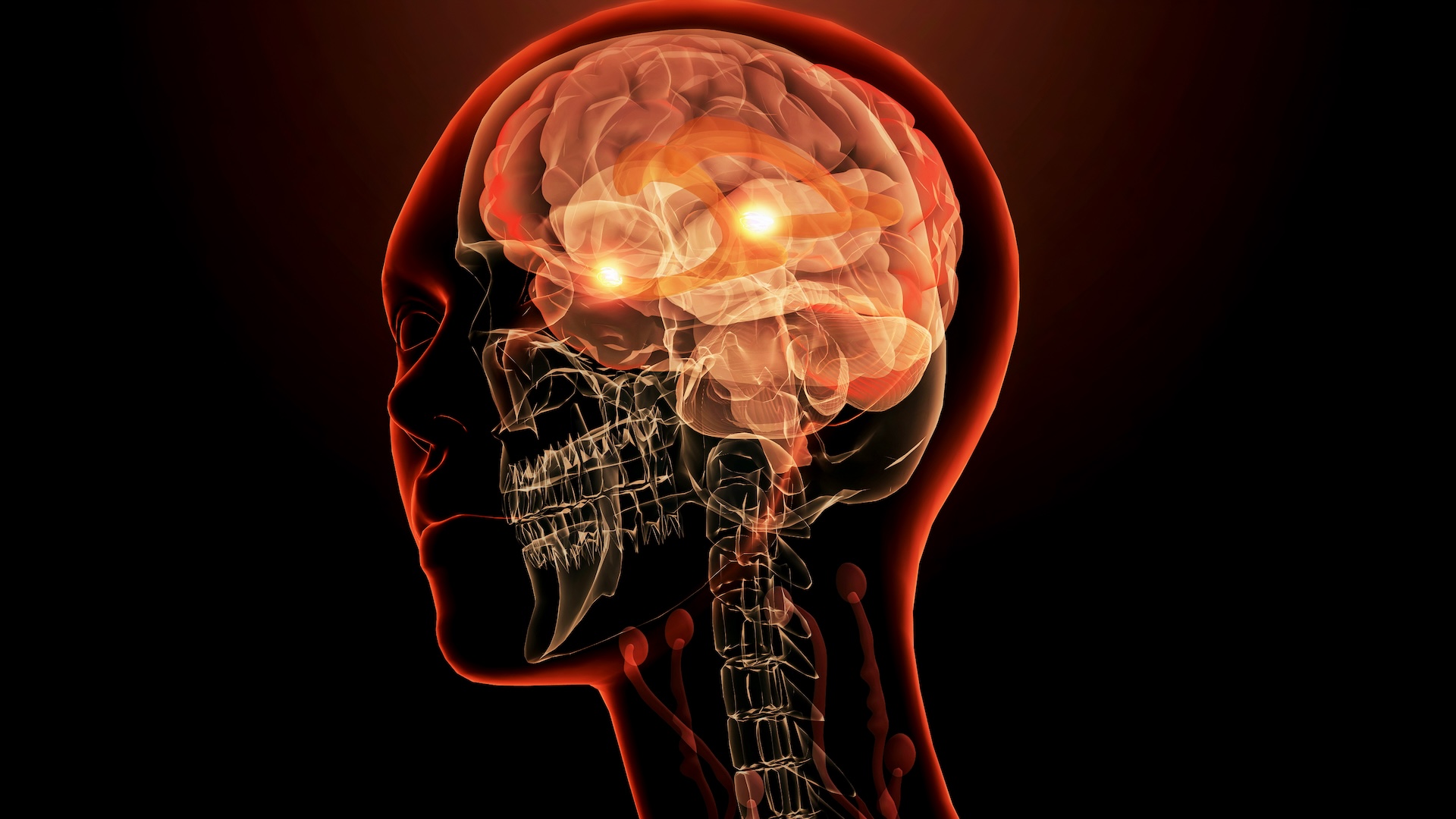
Scientists just discovered that the primary messengers controlling the brain's "fear circuit" aren't what we thought they were.
When you accidentally touch a pan on the stovetop or brush up against a scalding hot iron, you reflexively pull back with a feeling of pain and a sudden sense of danger. This is because the pain receptors in your hands shoot a signal through your spinal cord and brainstem, where a specific group of neurons then sends those signals to the brain's fear center, the amygdala. This triggers an emotional fear response that, in this case, helps us remember to avoid touching hot surfaces — but this fear-driven mechanism also comes into play in many other scenarios.
Our ability to respond to and create a threat memory following pain happens quickly, and it is an important survival mechanism. But in disorders such as post-traumatic stress disorder and severe anxiety, this fear and threat response can go haywire.
Existing treatments for these disorders are only partially effective at treating the symptoms and mainly focus on tweaking molecules known as "fast-acting neurotransmitters." These extra-speedy chemical messengers are generally accepted as the relayers of rapid responses, such as pain, fear and danger avoidance. But a recent study, published July 22 in the journal Cell, calls that into question.
Related: Traumatic memories are processed differently in PTSD
Sung Han, a faculty member at the Salk Institute, and his colleagues hypothesized that other molecules could be involved in rapid fear responses — specifically, they pointed to slower-acting molecules called neuropeptides. But the proper tools to study these molecules didn't exist.
For their study, the researchers developed a new system to identify and modulate neuropeptides in live mice, and they found that it was these slow-acting molecules, not the fast-acting neurotransmitters, that play a primary role in the fear response circuit.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The threat response is not what we thought
Information from the environment travels to our brain via neurons that act as circuits, guiding the signal to where it needs to go. A signal is passed along when one neuron sends molecules, such as neurotransmitters or neuropeptides, to the next neuron in line. Fast-acting neurotransmitters are released in small packages and can quickly bind to and open another neuron's ion channels — tunnels that allow charged particles to pass in and out of the cell. This chain reaction changes the chemistry of the cell and ultimately transmits the signal to the next neuron.
Unlike neurotransmitters, slow-acting neuropeptides are released in larger packages — called large dense core vesicles (LDCVs) — and bind to a specific receptor on the neighboring neuron. This jumpstarts a cascade of enzyme activity that triggers a flurry of gene activity.
According to Han, many believe these slow neuropeptides only have a role in modulating the fast neurotransmitters, not in signaling by themselves. But Han and his colleagues were not convinced and believed the molecules play an unsung role in shuttling messages through the nervous system.
They wanted to test whether neuropeptides can act like a primary neurotransmitter, as well as identify which ones are involved in the fear response.
"But there's no tool to test this idea," Han told Live Science. The researchers would need to monitor the release of the neuropeptides in cells or in living animals and then test whether those messengers alone are sufficient to deliver information, he said."
The researchers solved this problem by designing a tool that targets the LDCVs that transport neuropeptides. They created a sensor to detect when a LDCV is released from a cell, as well as a "silencer" that degrades specific neuropeptides when and where the scientists wanted. This enabled the researchers to see what happens in the brain when those neuropeptides are absent.
The use of a sensor for LDCV release in a living animal and the ability to silence neuropeptides is a novel idea, according to Dr. Robert Edwards, a faculty member at the University of California, San Francisco who was not involved in the work. "The role of many peptides remains poorly understood relative to classical transmitters, so this is largely uncharted territory," Edwards said.
Using their new tools, the researchers used lab mice to identify which neuropeptides were released when the rodents experienced various mild stimuli that elicit the fear response. One test used involved the mice experiencing a mild shock to their feet when they heard a specific sound; this conditioned the mice to freeze in place when they heard the noise.
The team looked at what happened when they silenced several neuropeptides in the mice, compared to when they switched off a neurotransmitter called glutamate. They were surprised to find that it was, in fact, the neuropeptides that were the main purveyors of the fear response, not glutamate.
They concluded this because switching off glutamate had no effect on the mice's fearful freezing behavior. However, turning off the neuropeptides suppressed that freezing behavior for a whole day.
"It was really surprising when we observed that the glutamate doesn't do anything," Han said. "So glutamate is the main molecule for neuronal communication. But at least in our case, glutamate doesn't do anything in terms of the threat signal information relaying to the amygdala."
The researchers also found that multiple neuropeptides were packaged into the same vesicle. When the researchers inhibited all these neuropeptides, they found they were able to reduce the mouse's fear response much more effectively than when they inhibited just one. Current treatments for fear and panic disorders typically target just one neurotransmitter, so this could provide a new path forward.
Han believes that designing molecules that target multiple neuropeptide receptors could result in more effective panic-disorder treatments.
"Targeting slow transmitter systems, especially the neuropeptide, for treating anxiety or PTSD or pain, I think, may be beneficial and may actually open new avenues for drug development," Han said.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Jennifer Zieba earned her PhD in human genetics at the University of California, Los Angeles. She is currently a project scientist in the orthopedic surgery department at UCLA where she works on identifying mutations and possible treatments for rare genetic musculoskeletal disorders. Jen enjoys teaching and communicating complex scientific concepts to a wide audience and is a freelance writer for multiple online publications.