Can viruses cause cancer?
The far-reaching impact of certain viruses on the body can make cells grow out of control, causing cancer.
Smoking, being exposed to toxic chemicals or radiation, and carrying mutations in certain genes are some of the best-known risk factors for cancer. But another cause of cancer isn't discussed as often: viruses.
So which viruses can cause cancer, and how do they do it?
There are at least seven viruses that are known to contribute to the development of cancer in humans, either directly or indirectly. These include human papillomaviruses (HPV), hepatitis B virus (HBV), hepatitis C virus (HCV), Epstein-Barr virus (EBV), Kaposi's sarcoma-associated herpesvirus, human T-cell lymphotropic virus and Merkel cell polyomavirus. In addition, human immunodeficiency virus (HIV) raises the risk of cancer in part by opening the door for cancer-driving viruses to invade the body.
It's important to note, however, that only a small percentage of people who are infected with these viruses go on to develop cancer — in other words, catching one of these viruses doesn't guarantee that you'll develop cancer. For example, over 90% of adults worldwide have been infected with EBV at some point in their lives, but only 1% of cancers are associated with EBV, the virus behind "mono."
Related: What's the oldest known case of cancer in humans?
Cases driven by all these viruses do add up, though. An estimate based on 2012 infection numbers suggested that viral infections may contribute to more than 1.4 million cancer cases worldwide that year, representing about 10% of all cancer cases.
"For a long time, many people in the field were very skeptical that any virus has caused cancer in people," Dr. Jay Berzofsky, a senior investigator at the National Cancer Institute, told Live Science. "And then, once there were some discovered, more people jumped on that bandwagon and found more."
Get the world’s most fascinating discoveries delivered straight to your inbox.
Berzofsky explained that viruses can have carcinogenic, or cancer-causing effects through both direct and indirect mechanisms, and each virus can cause cancer through a unique route.
Direct mechanisms
One of the best-known viruses that can cause cancer is HPV, a family of viruses that is responsible for more than 37,000 new cancer cases in the U.S. each year. The virus is known for its association with cervical cancer, but it can also cause anal, oropharyngeal (back of the throat), penile, vaginal and vulvar cancers.
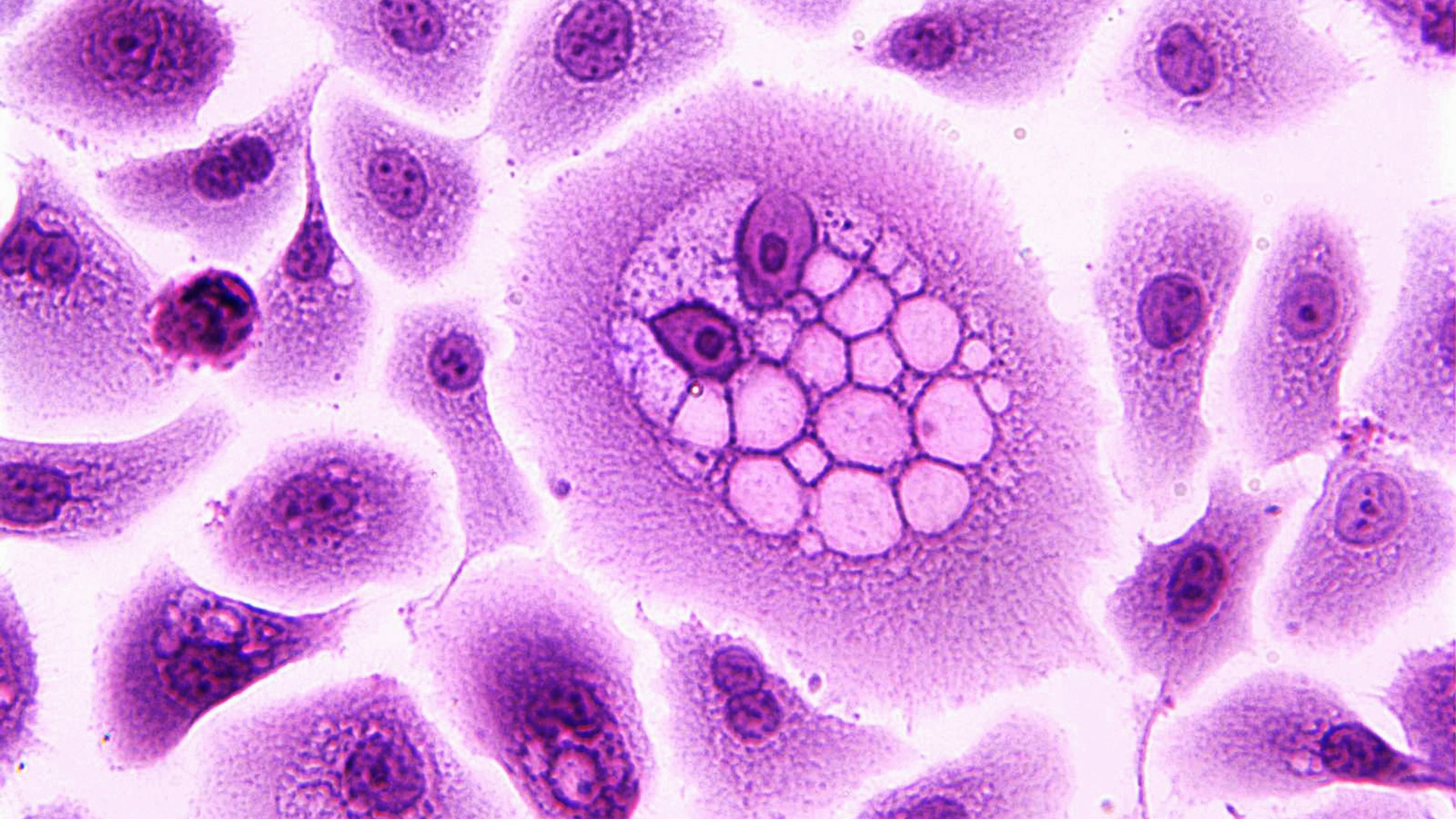
Certain HPV viruses promote cancer by transforming normal, healthy cells into abnormal, tumorous cells. This happens because HPV manufactures certain proteins, called E6 and E7 oncoproteins, that inactivate the natural tumor suppressor systems of healthy cells.
"That allows the abnormal cells to grow uncontrolled," Dr. Harrys Torres, a professor of infectious diseases at the University of Texas MD Anderson Cancer Center, told Live Science.
There are more than 200 types of HPV, but only 12 have been strongly associated with cancers. The HPV vaccine, which is recommended for all children between the ages of 11 and 12, protects against these high-risk forms of the virus that could lead to cancer. People can get the shot up to age 26 if they didn't previously receive all their recommended doses.
Other viruses that can directly cause cancer, like EBV and human T-cell lymphotropic virus, exert their effects through different cellular and genetic mechanisms. However, the result is ultimately similar: cancerous cells start to replicate aggressively and evade the body's natural defense systems.
Many factors influence whether infection with these viruses lead to cancer. In the case of HPV and EBV, certain strains have more cancer-causing potential than others. People with weakened immune systems are also at greater risk of developing virus-related cancers. And external factors, such as existing mutations or exposure to environmental carcinogens, can multiply the likelihood of tumor growth.
Related: New self-swab HPV test is an alternative to Pap smears. Here's how it works.
Indirect mechanisms
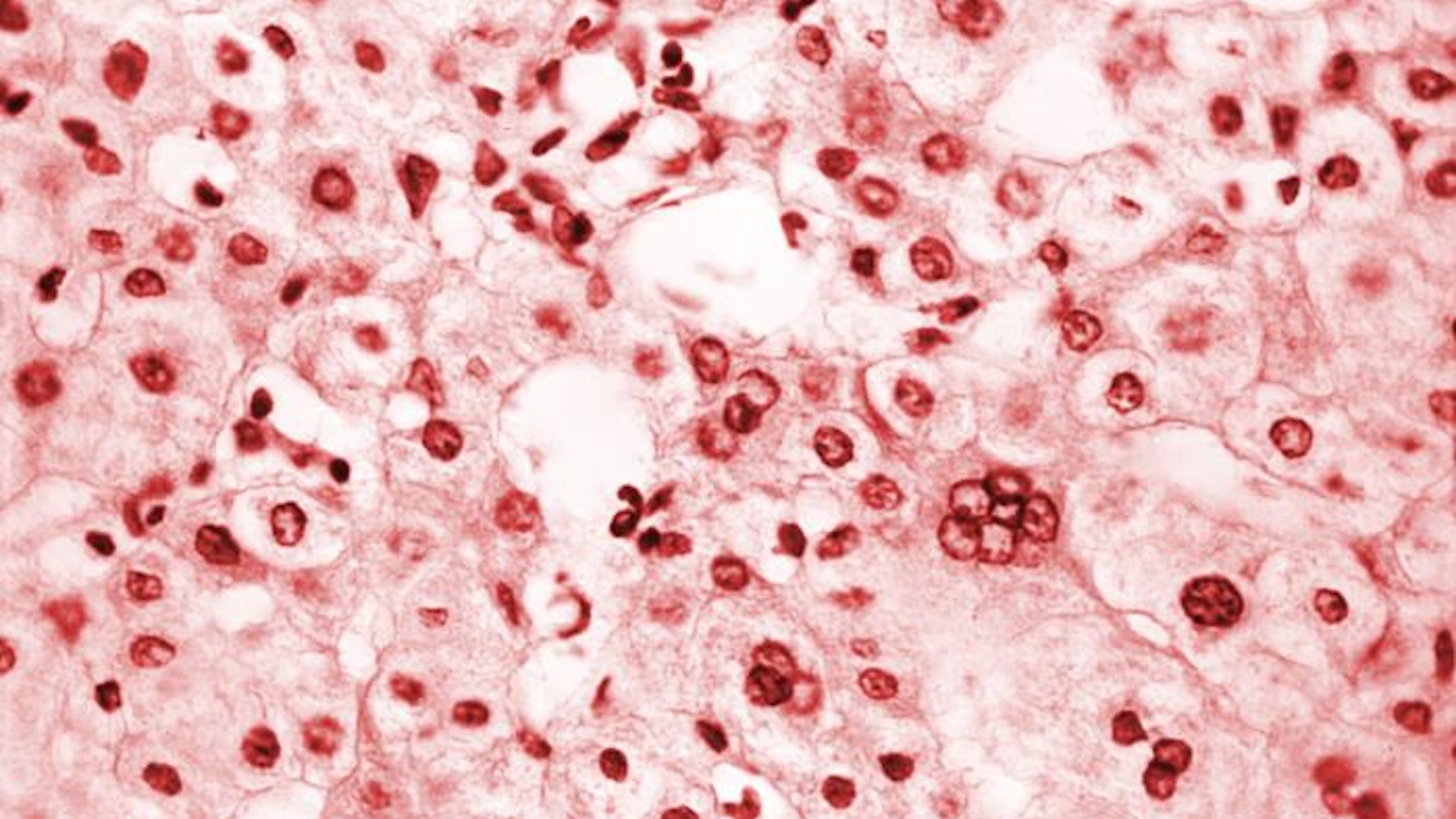
Viruses can cause cancer through more indirect mechanisms, too. Both HBV and HCV illustrate this. HBV and HCV infect the liver, which in the case of chronic infections, leads to long-term inflammation and cirrhosis, or scarring of the liver.
"Anything that causes chronic inflammation can potentially increase the risk of cancer," Berzofsky said.
As the body tries to repair the extensive damage from HBV or HCV by making new liver cells, there's a chance that some of those cells will mutate and become cancerous. HCV is also associated with non-Hodgkin's lymphoma, a cancer of the lymphatic system, possibly because the constant stimulation of the immune system caused by the virus spurs the development of cancerous cells.
HIV can also raise the risk of cancer developing through indirect mechanisms. That's because uncontrolled HIV infections cause chronic inflammation and weakens the immune system, which makes the body more susceptible to the other viruses directly associated with cancer.
Prevention is key
Although the ways these viruses can cause cancer can be complex and layered, Torres said there are methods for preventing and treating some of these infections.
There are vaccines against HPV and HBV, both of which are highly effective. For example, recent data found absolutely no new cases of cervical cancer in a large cohort of young women in Scotland who had received the HPV vaccine between the ages of 12 and 13.
Both HIV and HBV spread through multiple bodily fluids, such as blood and semen, while HCV primarily spreads through just blood. Using condoms and never sharing needles can help reduce the risk of contracting the infections, and preventative medicines called PrEP are also available for HIV. Note that these viruses can also spread to fetuses and newborns during pregnancy, childbirth or breastfeeding, so pregnant people are advised to get tested for the infections.
Antiviral treatments can also keep conditions like HIV and chronic HBV at bay, making them less likely to cause cancer. And HCV infections are curable with antivirals.
Torres is hopeful that vaccination, prevention and treatment of these viruses can help decrease the global cancer burden.
"It's a work in progress," he said. "We're trying to do as much as we can."

Marilyn Perkins is the content manager at Live Science. She is a science writer and illustrator based in Los Angeles, California. She received her master’s degree in science writing from Johns Hopkins and her bachelor's degree in neuroscience from Pomona College. Her work has been featured in publications including New Scientist, the Johns Hopkins Bloomberg School of Public Health magazine and Penn Today, and she was the recipient of the 2024 National Association of Science Writers Excellence in Institutional Writing Award, short-form category.