Chlamydia may hide in the gut and cause repeated infections
A mini model of the human intestines suggests that chlamydia bacteria can colonize the gut, potentially contributing to recurrent infections.
Get the world’s most fascinating discoveries delivered straight to your inbox.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered Daily
Daily Newsletter
Sign up for the latest discoveries, groundbreaking research and fascinating breakthroughs that impact you and the wider world direct to your inbox.

Once a week
Life's Little Mysteries
Feed your curiosity with an exclusive mystery every week, solved with science and delivered direct to your inbox before it's seen anywhere else.

Once a week
How It Works
Sign up to our free science & technology newsletter for your weekly fix of fascinating articles, quick quizzes, amazing images, and more

Delivered daily
Space.com Newsletter
Breaking space news, the latest updates on rocket launches, skywatching events and more!

Once a month
Watch This Space
Sign up to our monthly entertainment newsletter to keep up with all our coverage of the latest sci-fi and space movies, tv shows, games and books.

Once a week
Night Sky This Week
Discover this week's must-see night sky events, moon phases, and stunning astrophotos. Sign up for our skywatching newsletter and explore the universe with us!
Join the club
Get full access to premium articles, exclusive features and a growing list of member rewards.
The bacteria behind chlamydia can colonize the gut, and from that hiding place, they may act as a source of repeated infections, new research using miniature intestines suggests.
Chlamydia is the most common sexually transmitted infection (STI) worldwide. The form of the infection that affects humans is caused by a species of bacteria known as Chlamydia trachomatis.
The disease most often affects the genital region, sometimes causing pain and unusual discharge from the vagina or penis. However, over the years, research in mice and various clinical reports in humans have suggested that C. trachomatis may also be able to infect the human digestive tract. This means that, theoretically, the bacteria could hide in the gut and then cause repeated genital infections, which commonly occur in patients despite treatment with antibiotics.
Yet, until now, scientists haven't been able to test this theory in human cells.
Now, in a new study published Thursday (Aug. 22) in the journal PLOS Pathogens, researchers used miniature, lab-grown models of different parts of the human digestive tract to study whether C. trachomatis could indeed infect the gut.
To make these models, the team used chemicals to coax stem cells taken from adult donors to grow into miniature, 3D replicas of full-size organs. These included the large and small intestines. These types of tiny models, known as "organoids," have become an increasingly popular tool for scientists to study physiological systems and to test new drugs. Organoids can be made to more accurately recapitulate the structure and function of human organs, compared with other cell-based or animal models.
Get the world’s most fascinating discoveries delivered straight to your inbox.
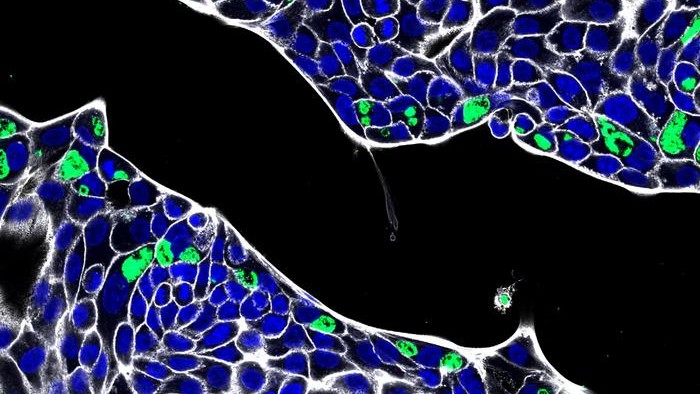
Once the digestive organoids had grown to a large enough size, the researchers extracted specific cells called primary intestinal epithelial cells, which line the surface of the intestines. They then grew these cells in single layers in a lab dish, to expand their numbers, before infecting them with C. trachomatis. They zoomed in on this interaction under a high-resolution microscope.
The researchers showed that C. trachomatis was able to enter the cells. In some cases, the development of the bacteria was restricted, so instead of causing a full-blown infection, C. trachomatis formed large, irregularly-shaped structures called aberrant bodies. These aberrant bodies are thought to be able to persist within host cells in the body.
"The intestine could represent an overlooked site of infection where chlamydia could potentially persist and repeatedly spread to the genital tract," Pargev Hovhannisyan, lead study author and a doctoral student at the University of Würzburg in Germany, told Live Science in an email.
"If so, this could compromise the success of the antibiotic treatment for genital infections."
In a separate experiment, the team also showed that C. trachomatis relied on a ringlet of DNA, known as a plasmid, to infect and grow within epithelial cells. This plasmid is known as Pgp3 and is made by the bacteria itself. After trying and failing to infect cells with modified strains of the bacteria that didn't carry Pgp3, the team realized the microbe's reliance on the plasmid.
The team acknowledged several limitations of the study, including that they looked only at how C. trachomatis infects isolated epithelial cells, rather than those embedded in an organoid. There are many factors in the human gut, such as other microbes and cells of the immune system, that could help thwart infection of these cells in real life, they noted. Therefore, it's still not completely certain that these infections happen in human patients.
Nevertheless, the models that the scientists created should help facilitate future research into the possible role of chlamydia infection in the gut, the team said.
Editor's Note: This story was updated on Aug. 27, 2024 to add a quote from Pargev Hovhannisyan. The original article was published on Aug. 22, 2024.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30.
 Live Science Plus
Live Science Plus