'Mind-control' parasite Toxoplasma hides from the immune system with 2 key genes
A single-cell parasite relies on two genes that boost each other's activity to switch into "defense mode" when attacked by the immune system.
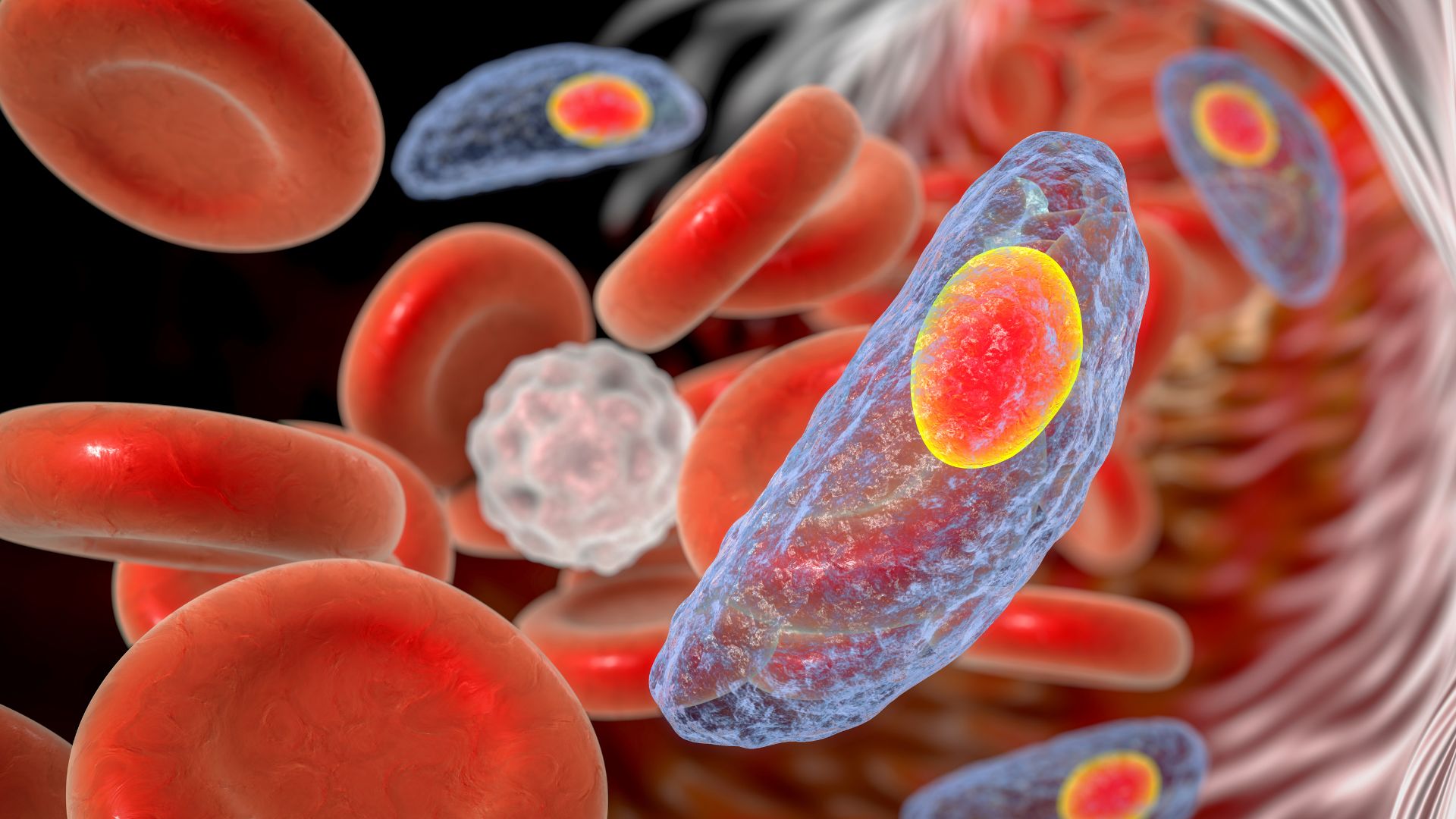
The parasite Toxoplasma gondii hides in up to half of humans, although it rarely causes symptoms. But when it infects mice, the single-cell organism can exert a kind of "mind control" to change the rodents' behavior and help itself spread.
Now, researchers report being one step closer to curing T. gondii infections in humans, which can be lifelong due to the parasite's ability to morph into a dormant, defensive state. Two transcription factors — proteins that switch genes "on" and "off" — lie at the root of this metamorphosis, and the discovery opens avenues to block the process.
Often dubbed the "mind-control parasite," T. gondii takes over the minds of infected mice and steers them towards cats to become their next meal. This enables the parasites to jump into our feline friends, the only known hosts in which they can reproduce sexually.
Scientists remain unsure whether the parasite can similarly control the human brain; some studies suggest it could contribute to aggression, impulsive behavior and schizophrenia, while other studies dispute these effects. Most people carrying T. gondii don't develop any symptoms, but more rarely, the infection can trigger mild, flu-like symptoms or even severe illness. Developing fetuses, newborns, and people with weak immune systems are most vulnerable to severe toxoplasmosis, which can damage the eyes and brain and sometimes be fatal.
Related: Can a cat parasite control your mind?
The parasite proliferates rapidly in its "tachyzoite" form. But under stressful conditions like an immune attack, T. gondii burrows into brain and muscle tissue and morphs into a "bradyzoite," which encloses itself inside a cyst and waits to revert to its active state. Immune cells and current treatments can clear away tachyzoites, but the cysts protect the bradyzoites from attack.
Parasitologist Sebastian Lourido and his colleagues at Massachusetts Institute of Technology (MIT) previously discovered a protein that switches "on" genes essential for turning tachyzoites into bradyzoites, which they named Bradyzoite-Formation Deficient 1 (BFD1). However, the regulation of BFD1 remains poorly understood.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
In the new study published April 20 in the journal Nature Microbiology, the team discovered another transcription factor that regulates BFD1, which they named BFD2.
The study "mechanistically added a lot" to the initial story, said Mohamed-Ali Hakimi, a parasitologist at Grenoble Alpes University in France who was not involved with the work.
When the researchers deleted the gene that codes for BFD2, they found that tachyzoites could not switch into bradyzoites and form cysts. The scientists injected 100 copies of the parasite without the gene into mice and didn't detect cysts in brain autopsies performed 45 days later. This couldn't be explained by the immune system successfully clearing away the parasite because low levels of tachyzoites were still detected.
Next, the team determined that BFD1 and BFD2 regulate each other. Stress boosted both BFD1 and BFD2 in mice, but deleting the BFD1-coding gene also silenced the gene for BFD2. The researchers determined that BFD1 binds to the BFD2-coding gene and switches it "on."
BFD2 regulates BFD1 differently, however. When the gene for BFD2 was deleted, the BFD1-coding gene remained "on," and its genetic instructions were copied down into mRNA molecules, which are needed to synthesize the BFD1 protein. However, no protein was produced.
The team determined that T. gondii cells maintain a supply of this mRNA, but they can only make the BFD1 protein when BFD2 binds to the mRNA and thus triggers protein synthesis. This binding only happens when the cell is under stress.
By perpetuating each other's activity, the two transcription factors can commit tachyzoites to morphing into bradyzoites by "locking the cell into this developmental trajectory," said M. Haley Licon, parasitologist and lead author of the study. Future research could unravel what factors switch "off" this self-perpetuating loop, she added, enabling bradyzoites to revert to tachyzoites when stressful conditions elapse.
"We still don't know what the signals that control differentiation are," Lourido told Live Science in an email. Unraveling those signals may be key to halting bradyzoite formation, he added.
"Current therapies against Toxoplasma cannot cure the infection because the chronic stages are resistant," Lourido explained. He added that inhibiting differentiation could render the parasite "susceptible to existing drugs," which could cure the infection.
Hakimi argued that scientists are a long way from developing such drugs. "It's very hard to target transcription factors," and aside from select drugs used in cancer treatment, "very few drugs" do, he said.
Licon agreed but is optimistic that "understanding the circuit and regulation thereof" could reveal ways to block the parasite from entering its protected, dormant state.

Kamal Nahas is a freelance contributor based in Oxford, U.K. His work has appeared in New Scientist, Science and The Scientist, among other outlets, and he mainly covers research on evolution, health and technology. He holds a PhD in pathology from the University of Cambridge and a master's degree in immunology from the University of Oxford. He currently works as a microscopist at the Diamond Light Source, the U.K.'s synchrotron. When he's not writing, you can find him hunting for fossils on the Jurassic Coast.
Flu: Facts about seasonal influenza and bird flu
What is hantavirus? The rare but deadly respiratory illness spread by rodents










