New cause of asthma lung damage revealed
In a lab study, scientists have pinpointed a potential way to "break the inflammatory cycle" of asthma.

Scientists may have uncovered an overlooked factor in why asthma attacks happen, and they say it could open up a whole new avenue for treatments.
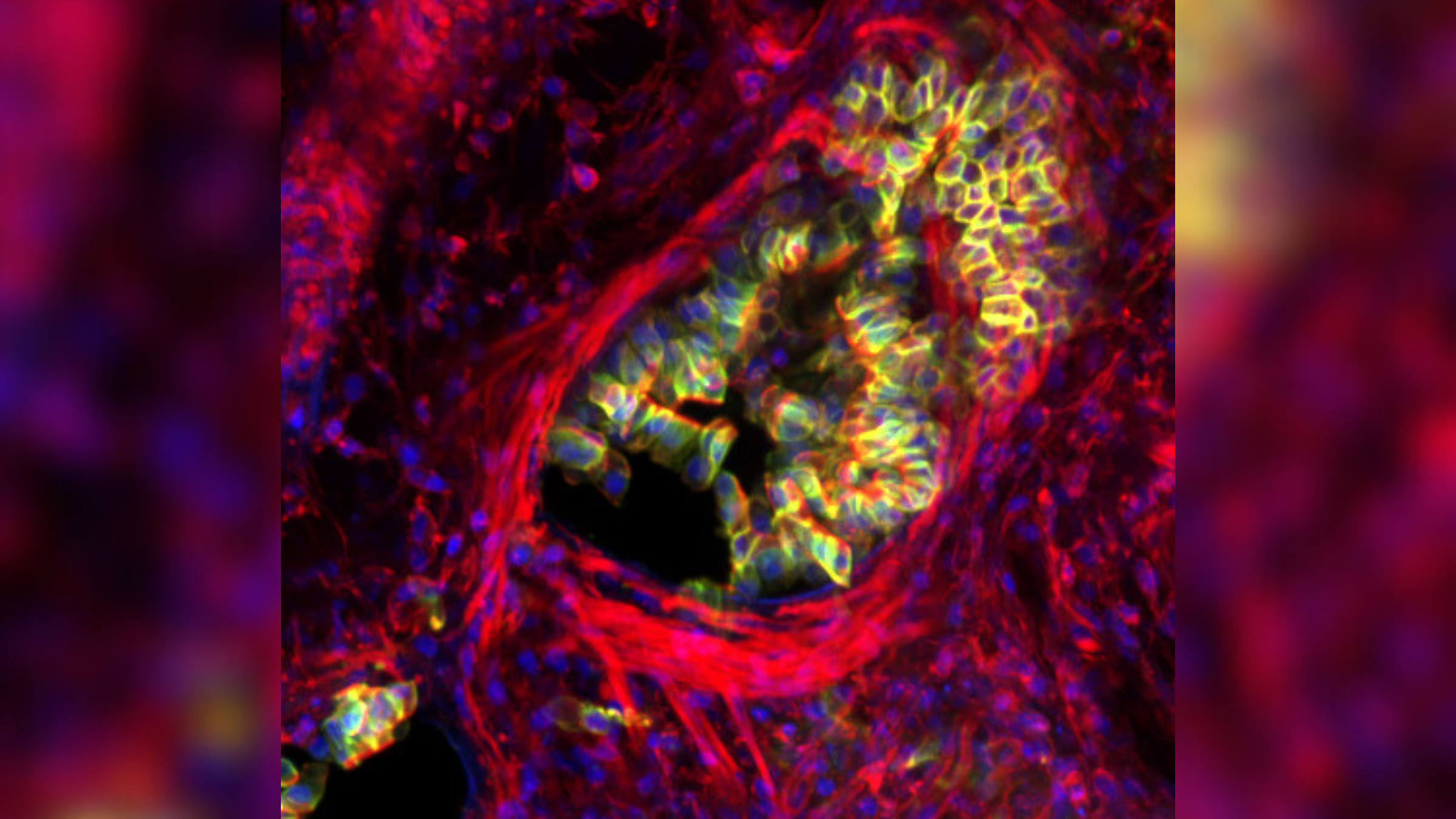
In a laboratory study in mice and human tissues, the researchers revealed how asthma attacks kill cells in the airways of the lungs. They found that when the airways constrict during an asthma attack, the thin layer of cells that line these passageways — called epithelial cells — becomes too crowded, causing some cells to be squeezed out of the tissue and die.
As a result, this protective barrier in the lungs becomes damaged, triggering inflammation and mucus secretion that blocks the airways and hinders breathing, according to the new research, published April 4 in the journal Science.
"Without this barrier, asthma sufferers are far more likely to get long-term inflammation, wound healing, and infections that cause more attacks," Jody Rosenblatt, co-senior study author and a professor of cell biology at King's College London, said in a statement. That's partly because, without the barrier, allergens and irritants can reach places in the lungs that they might not otherwise be able to get to.
Related: Asthma drug omalizumab approved for severe food allergies
In their experiments, the researchers also found ways of stopping this chain reaction and keeping cells in their place in the lung tissue. This treatment approach "may have the capacity to break the inflammatory cycle and potentially revolutionize how asthma is treated," Dr. Jeffrey Drazen and Jeffrey Fredberg of the Harvard School of Public Health wrote in a commentary of the study.
Current treatments for asthma manage only its symptoms. For instance, the drug albuterol opens up the airways during an attack, while inhaled corticosteroids calm inflammation to reduce the chances of having an attack. The drugs don't prevent attacks by addressing their underlying causes.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Having a better understanding of how asthma attacks happen could lead to new therapies for the disease, Chris Brightling, co-senior study author and a professor of respiratory medicine at the University of Leicester in the U.K., said in the statement.
To gain this understanding, Brightling and colleagues mimicked asthma attacks in the lab by treating lung tissue from mice with a chemical that triggers constriction in muscle cells that line the airways. Under the microscope, they saw that this constriction causes epithelial cells to be squeezed out of place and die, and this triggered the characteristic inflammation and mucus secretion that occurs during asthma attacks.
These features were also seen in tissue samples from human patients with asthma who had been treated with corticosteroids. The finding reinforced the idea that cell squeezing underlies the pathology of the disease.
In previous work, the team discovered that a colorless fluid called gadolinium, which is normally used to improve the clarity of magnetic resonance imaging (MRI) scans, could stop epithelial cells from being squished out of place.
In the new study, they found gadolinium was able to prevent epithelial cell damage, inflammation and mucus secretion in the mouse lung tissue, suggesting that it could be a new treatment option for asthma in people.
However, more research is needed to translate these findings into new-and-improved asthma treatments for the many people with the disorder.
Around 1 in 12 people in the U.S. have asthma. Common symptoms of the chronic condition include coughing, chest tightness, wheezing and shortness of breath. Asthma attacks occur when these symptoms suddenly worsen or become severe, which can be life-threatening.
In addition, this newfound knowledge could also one day lead to new treatments for other inflammatory diseases that may be partly caused by excessive muscle constriction, such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), the authors wrote in the paper.
Drazen and Fredberg agreed, writing that "such a mechanism helps to paint a more complete picture of asthma pathobiology and may be relevant to other conditions, such as irritable bowel syndrome, in which epithelial cells are subject to disruptive mechanical forces."
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to community@livescience.com with the subject line "Health Desk Q," and you may see your question answered on the website!

Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking NCTJ journalism training with News Associates. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. (emily.cooke@futurenet.com)









