Severe COVID-19 may shrink cancer tumors, early data suggest
Immune cells produced during severe COVID-19 infection may shrink tumors. The unexpected mechanism offers a new therapeutic possibility for advanced and treatment-resistant cancers.
Immune cells produced during a severe COVID-19 infection may cause cancerous tumors to shrink, research in mice suggests.
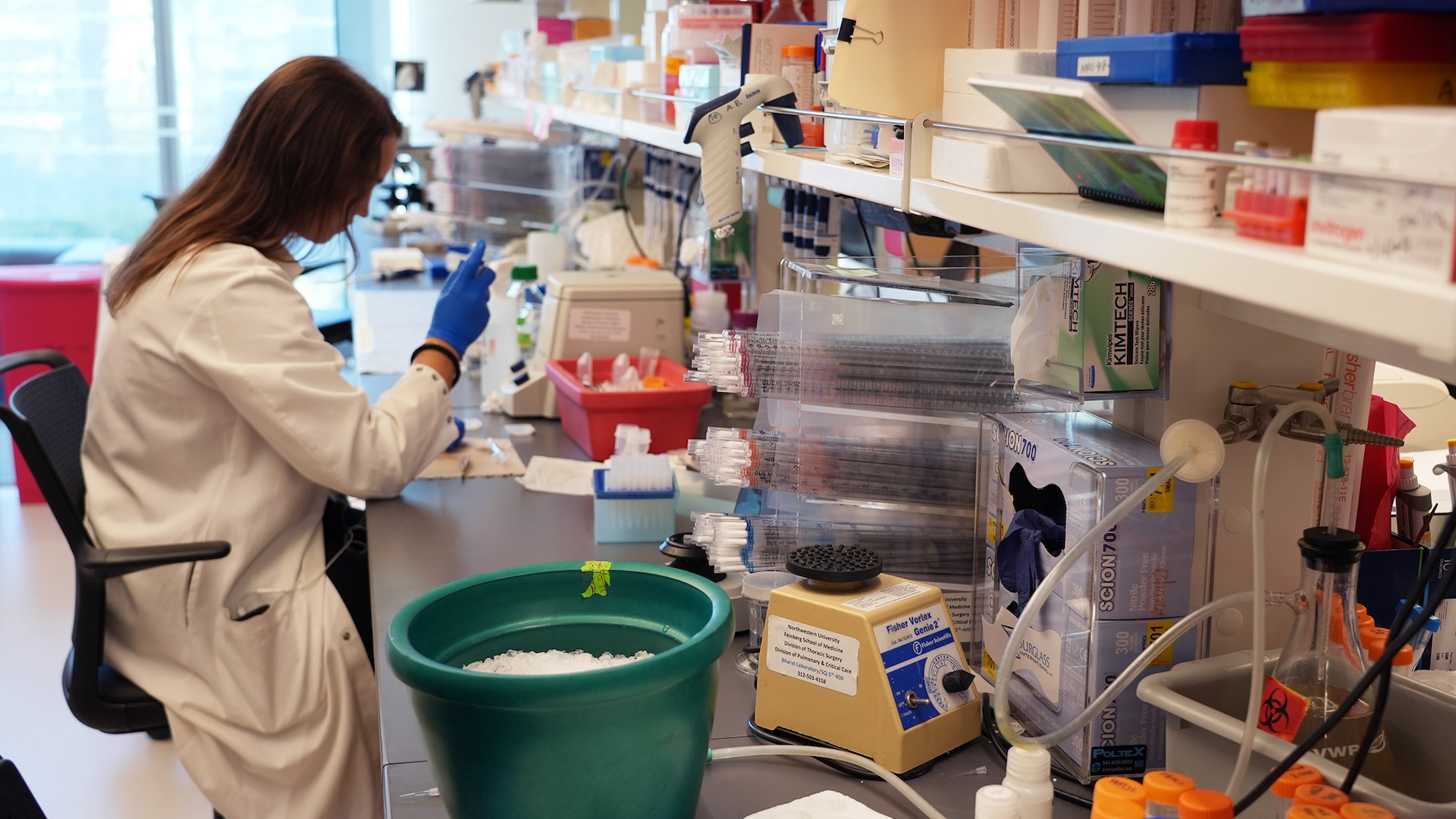
The study, published Friday (Nov. 15) in The Journal of Clinical Investigation, found that genetic information from the virus that causes COVID-19 led the immune system to produce special cells with anti-cancer properties. These immune cells, a type of white blood cell called monocytes, helped shrink several types of cancer in mice.
Normally, cancer spreads when monocytes assemble at a tumor site. The tumor cells then convert these monocytes into cancer-friendly cells, said study lead author Dr. Ankit Bharat, chief of thoracic surgery at Northwestern Medicine. These monocytes then help shield the cancer cells from the immune system, allowing tumors to grow.
"They essentially form like a castle around the cancer cells, protecting them from being invaded by the body's immune system," Bharat told Live Science.
Past research has shown that certain inflammatory conditions, such as COVID-19, can induce changes in monocyte properties. These "induced" monocytes are trained to specifically target the virus to orchestrate a more effective immune response, said Dr. Christopher Ohl, an infectious-disease specialist at Atrium Health Wake Forest Baptist and a professor at Wake Forest University School of Medicine in Winston-Salem, North Carolina, who was not involved in the study.
Bharat and his colleagues had noticed that some patients who had both severe COVID-19 and cancer had their tumors shrink after infection.
So they analyzed blood samples from people who had had a bout of severe COVID-19 and found that monocytes produced after severe infection retained a special receptor that bound well to a specific sequence of COVID-19 RNA.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
“If the monocyte was a lock, and the COVID RNA was a key, then COVID RNA is the perfect fit,” Bharat said.
The researchers also looked at mice with different types of Stage 4 cancer tumors — melanoma, lung, breast and colon cancer. The mice were given a drug to induce the monocytes and thus mimic the immune response to COVID-19 infection. The tumors shrank for the four types of cancer studied.
The researchers saw that the transformed monocytes had cancer-fighting properties. These induced monocytes are also not converted by tumors into "cancer-friendly" cells that shield tumors.
Instead, the transformed monocytes migrated to the mice’s tumor sites — something most immune cells cannot do. Once near the tumor, the monocytes activated natural killer cells. The killer cells then attacked the cancer cells, causing the cancer to shrink, Bharat said.
Bharat thinks the mechanism may work in humans and against other types of cancer as well since it disrupts a way most cancers spread throughout the body. "By activating this pathway, we precondition the monocytes to never become the cancer-friendly cells," Bharat said.
The COVID-19 vaccines on the market are unlikely to trigger this mechanism, since they do not use the same RNA sequence that the virus does, Bharat said. But future drugs and vaccines could be developed to spur the development of cancer-fighting monocytes, he added.
Importantly, the mechanism provides a new therapeutic possibility for advanced cancers that don't respond to approaches such as immunotherapy, which rely on the body's immune system to fight cancer.
While immunotherapy works roughly 20% to 40% of the time, it can fail if the body can't produce enough functioning T cells, which destroy cancer cells, said Dr. Yibin Kang, a professor of molecular biology at Princeton University, who was not involved in the study. For instance, a 2021 study in the British Journal of Cancer found that less than 15% of cancer patients saw an "effective anti-cancer immune response" from immunotherapy drugs alone.
"The problem [with current immunotherapy] is the reliance on T cell immunity against cancer," Kang told Live Science.
The current study is promising because it proposes a way to selectively kill tumors that is independent of T cells, Kang said.
Ohl agreed, saying the mechanism is a "detour" that bypasses traditional roadblocks encountered during immunotherapy.
Still, clinical trials are needed to determine whether the mechanism produces the same cancer-fighting effect in humans.

Julie Goldenberg is a journalist based in New York City. She was a former associate editor at AARP where she reported on aging in America. Her work has appeared in AARP the Magazine, AARP.org, and Forbes. She holds a Master of Science degree in Journalism from Columbia University's Graduate School of Journalism and a Bachelor's degree in psychology from McGill University.
Flu: Facts about seasonal influenza and bird flu
What is hantavirus? The rare but deadly respiratory illness spread by rodents