What happens to the body during an asthma attack?
Learn what happens inside the body during an asthma attack and why treatments help prevent or reverse the effects.

An asthma attack is a sudden worsening of asthma symptoms caused by inflammation and a narrowing of the airways. This can make breathing difficult and, in severe cases, be life-threatening.
Asthma affects hundreds of millions of people worldwide, and attacks can be triggered by allergens, respiratory infections, cold air, exercise or irritants, such as smoke and pollution. But what actually happens inside the body during an asthma attack?
"There are two key physiological changes during an asthma attack," said Dr. Allen Dozor, a professor of pediatrics and division chief of pulmonology, allergy and sleep medicine at New York Medical College.
The first is bronchospasm, Dozor told Live Science. During an asthma attack, the bronchi of the lungs — the passages that connect the windpipe to the lungs — spasm and narrow, making it difficult to breathe.
Related: Could allergies be 'deleted' someday?
The second change, he said, is inflammation in the airways, which is how the body reacts to allergens or pollutants we breathe in. "Inflammation is quite complicated, but we now recognize that some patients with asthma have very mild inflammation and some have massive inflammation," Dozor clarified.
In addition to bronchospasm and inflammation, mucus production can play a role in asthma. The lungs produce thick mucus, which clogs the narrowed airways and makes breathing more difficult. People with asthma typically experience ongoing airway inflammation, which leads to chronically elevated mucus production, as well as a thickening of the airway lining over time. Plus, during an asthma attack, there is a short-term surge in mucus production triggered by inflammatory chemicals and molecules, such as histamine and leukotrienes, which are made by immune cells.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
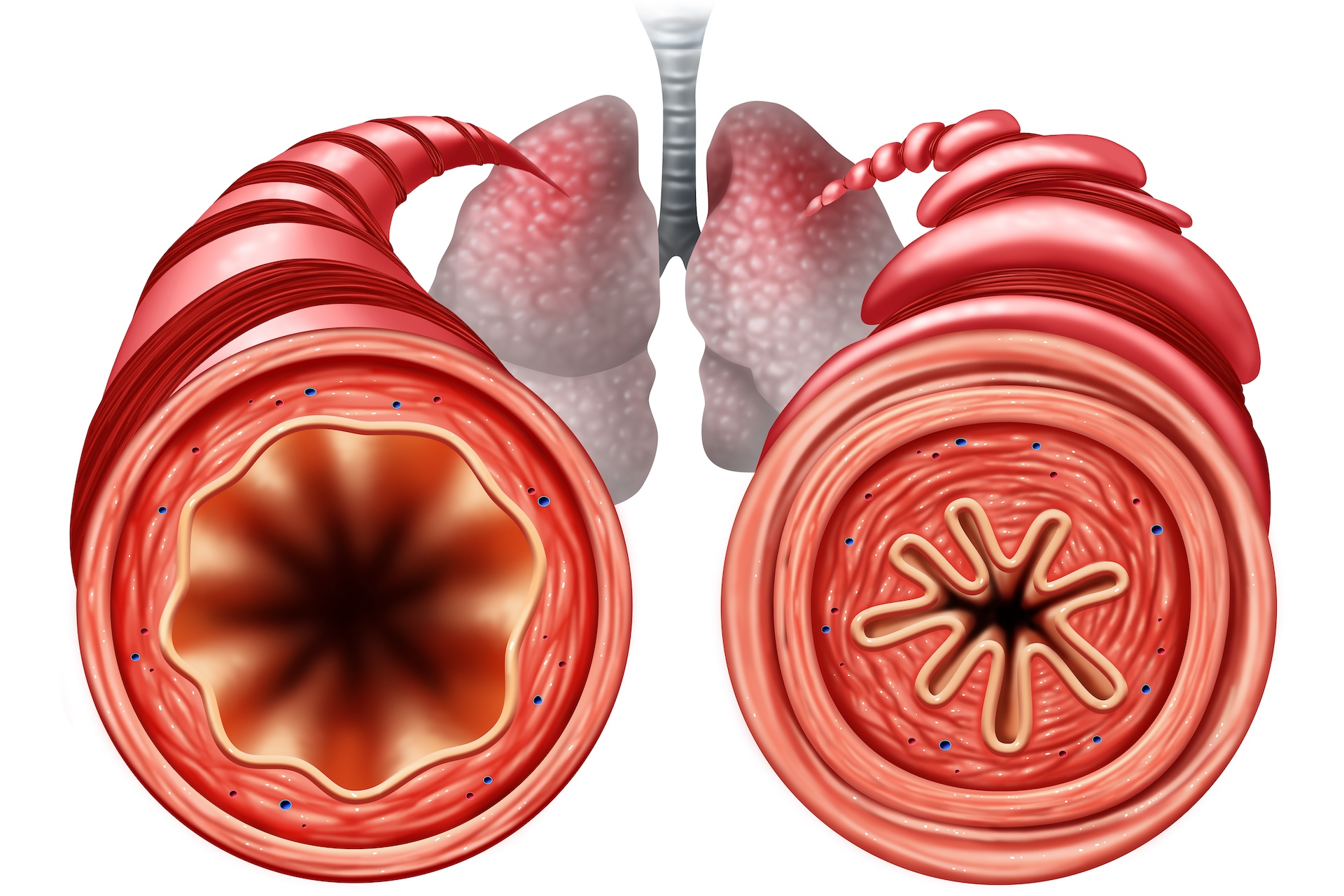
These three factors — bronchospasm, inflammation and mucus — combine to make breathing labored, leading to the hallmark symptoms of an asthma attack, including wheezing, shortness of breath, coughing and chest tightness.
When the airways begin to close, the body struggles to get enough oxygen. In mild cases, this may result in breathlessness and coughing, but in more severe attacks, oxygen levels can drop significantly, leading to dizziness, confusion and even a loss of consciousness. If untreated, a severe asthma attack can be fatal.
The most immediate treatment for an asthma attack is a rescue inhaler, which typically contains albuterol, a compound that quickly relaxes the airway muscles and stops the release of some chemicals involved in the hypersensitivity reaction. For more severe cases, corticosteroids, which suppress inflammation, may be given orally or through an IV. In emergency situations, oxygen therapy or mechanical ventilation may be required to help people breathe.
Prevention of asthma attacks involves avoiding the triggers of these three mechanisms that drive people's symptoms.
"Prevention is one of the most important aspects of asthma care," Dr. James Lyons, a family medicine physician with expertise in asthma and a medical consultant for Synergy Houses, told Live Science in an email. "The best way to avoid severe attacks is to identify and minimize exposure to triggers, whether allergens, smoke, cold air, or strong odors."
Additionally, preventive medications that control asthma lower the risk of bronchospasm, inflammation and mucus production. These include inhaled corticosteroids, to snuff out inflammation and help counter mucus production, and long-acting beta-agonists, which help relax the airways. Some inhalers combine multiple medications to help stave off attacks.
"Sticking to a prescribed medication regimen — especially for those with persistent asthma — is also key," Lyons said.
Disclaimer
This article is for informational purposes only and is not meant to offer medical advice.

Caleb Neal studied biomedical sciences and Spanish at the University of Rhode Island for undergraduate studies and then received a Masters of Public Health (MPH) degree from Augusta University. He's currently in his final year of medical school at New York College of Osteopathic Medicine (NYITCOM) and applying for residency in Emergency Medicine for 2025. He also worked for several years for Community Healthcare Network (CHN) a public health non-profit in New York City, helping conduct research and connect patients to social services.
- Nicoletta LaneseChannel Editor, Health
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.









