The new coronavirus has upended all of our usual calculus about seemingly ordinary activities. Is running past someone on the street safe? How about shopping in a grocery store with a 6-foot (2 meters) distance? And what about packages and takeout? And which of these activities poses the biggest risk?
Unfortunately, there's a lot we still don't know about the way the virus that causes COVID-19 spreads.
"At this point, I don't think anyone can take a group of people with COVID, say how each person has become infected, and then say that xx% got infected with droplets and yy% got infected via touching surfaces," Dr. Jeffrey N. Martin, a professor in the Department of Epidemiology and Biostatistics at the University of California, San Francisco, told Live Science in an email. "I don't think this kind of study has ever been done for any infection. In most individual persons, we do not know how the person got infected."
Related: Live updates on COVID-19
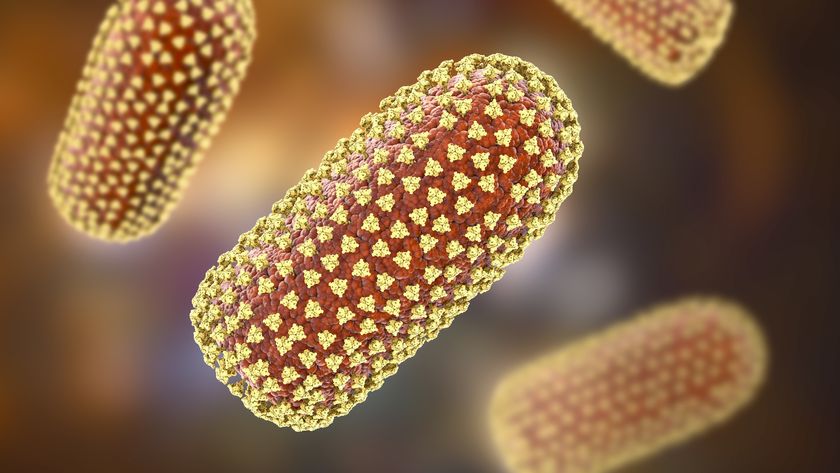
But as time goes on, we're learning more. Here's what we do know about how the new coronavirus, SARS-CoV-2, spreads.
Respiratory transmission
While the basic outlines of disease transmission have not been upended by COVID-19, there are some nuances that could play an important role in the spread of the disease. From the beginning, the Centers for Disease Control and Prevention (CDC) have said that SARS-CoV-2 is a respiratory virus, and as such, it is mainly transmitted between people through "respiratory droplets" when symptomatic people sneeze or cough. This idea, that large droplets of virus-laden mucus are the primary mode of transmission, guides the CDC's advice to maintain at least a 6-foot distance between you and other people. The thinking is that gravity causes those large droplets (which are bigger than about .0002 inches, or 5 microns, in size) to fall to the ground within a distance of 6 feet from the infected person.
But that 6-foot guideline is more of a ballpark estimate than a hard and fast rule, said Josh Santarpia, the research director of Countering Weapons of Mass Destruction Program at the University of Nebraska's National Strategic Research Institute.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
"There really isn't anything magic about standing 6 feet away from someone that you are interacting with directly. If you stand talking to someone who is infected with the virus, whether it's 3 feet or 6 feet, there is going to be some risk of infection," Santarpia told Live Science in an email.
That's because even large respiratory droplets can travel fairly far if the airflow conditions are right, Santarpia said.
And some experts believe the 6-foot rule is based on outdated information.
"6 feet is probably not safe enough. The 3-6 foot rule is based on a few studies from the 1930s and 1940s, which have since been shown to be wrong — droplets can travel farther than 6 feet," said Raina MacIntyre, a principal research fellow and professor of global biosecurity, who heads the Biosecurity Program at the Kirby Institute, in Australia. "Yet hospital infection control experts continue to believe this rule. It's like the flat Earth theory — anyone who tries to discuss the actual evidence is shouted down by a chorus of believers.”
Another complicating factor is that at least 25% of the people who are transmitting the virus may be asymptomatic at the time, said Dr. Robert Redfield, director of the Centers for Disease Control and Prevention, Live Science previously reported. That suggests coughs and sneezes aren't necessary to transmit the virus, though it's not clear whether simply breathing spreads the virus, or whether talking is required.
Aerosol transmission
In order for the virus to be spread without being coughed or sneezed in large drops of mucus, it has to somehow be able to suspend in the air for long enough to infect passersby. And that’s another complicating factor in figuring out transmission: People emit virus particles in a range of sizes, and some are small enough to be considered aerosols, or fine particles that can stay suspended in the air for hours and can travel with air currents across tens of feet. A study published March 17 in the New England Journal of Medicine found that virus particles that were aerosolized could remain viable for up to 3 hours.
What's not clear from this data is whether the virus is commonly transmitted via aerosols, or how long the virus remains infectious in aerosols in real-world settings. In that study, researchers used an extremely high concentration of virus particles, which may not reflect those shed by people with the disease.
"To my knowledge, there is no definitive evidence of transmission where aerosol was the only possible route," Santarpia told Live Science. (For instance, even someone who's not sneezing may emit respiratory droplets when talking, because people may spit when talking, and those droplets could be deposited on surfaces.)
One case study is suggestive however; a choir group in Skagit, Washington, met for a two-hour practice in early March. No one was symptomatic, so singers weren’t coughing or sneezing out infected droplets. And everyone kept their distance. But when all was said and done, 45 people became infected with COVID-19 and at least two people died from the virus, the Los Angeles Times reported. That suggested the viral particles were shed as aerosols by someone, before being inhaled or otherwise acquired by other choir members. A 2019 study in the journal Nature Scientific Reports found that people emit more aerosol particles when talking, and that louder speech volumes correlate to more aerosol particles being emitted.
That case, along with those studies, suggest that the virus can be routinely transmitted via aerosols, though other routes of transmission (such as large droplets being emitted during singing or speech) are still possible explanations. In the 2003 SARS outbreak, aerosol transmission occurred during hospital procedures that generated large volumes of aerosols, such as intubation.
Contact transmission
There's one other route that's thought to play a role in the spread of COVID-19: contact transmission. In that situation, viral particles emitted from the respiratory tract of an infected individual land on a surface. Then, another person touches that object, then touches their nose, mouth or eyes. The virus then sneaks into the body via the mucous membranes, infecting the second person.
So far, no one knows how common this mode of transmission is, but it does seem to be possible. One study found that SARS-CoV-2 could remain viable on surfaces such as cardboard for up to 24 hours, and on plastic and steel for 2 to 3 days.
Santarpia has studied viral surface contamination in the context of patients hospitalized with COVID-19 at the University of Nebraska Medical Center. In that study, which was published March 26 on the preprint database medRxiv, Santarpia and his colleagues found viral contamination in air samples, on surfaces such as toilets, and on frequently touched surfaces. Also on March 26, the CDC published a report on the coronavirus-stricken Diamond Princess cruise ship. An investigative team found traces of RNA from SARS-CoV-2 on surfaces throughout the cruise ship, in the cabins of both symptomatic and asymptomatic infected passengers, up to 17 days later — though no evidence suggests this viral RNA was still infectious. (SARS-CoV-2 is an RNA virus, meaning its main genetic material is RNA, not DNA.)
Another case report published by the CDC — this time from Singapore — also suggests contact with contaminated surfaces can transmit the virus. In that case, a person who was infected with SARS-CoV-2, but not yet symptomatic, attended a church service. Later in the day, another person sat in the same seat, and also came down with COVID-19. Whether the virus was contracted via a contaminated surface, or potentially a lingering aerosol, however, couldn't be ascertained.
Is food safe?
So far, there's no evidence that the virus is transmitted via food. The virus will not live long in food proper, and while it's possible that food packaging from groceries or takeout could contain small concentrations of virus particles, it is easy to mitigate this risk by washing your hands after handling groceries or takeout, Ben Chapman, a professor and food safety specialist at North Carolina State University, previously told Live Science.
Related: How to shop for groceries during the COVID-19 pandemic
The takeaway?
The fact that so many seemingly innocuous activities can transmit the virus can be scary. And it can be even scarier not knowing the actual risks associated with each transmission route — without that information, how can we take the right steps to protect ourselves?
But ultimately, there's some reassurance in the data as well.
"What is true is that persons who have a member of their household infected with the virus have a higher probability of getting infected with COVID than people who do not have a member of their household infected. This tells us a lot. This tells us that close contact is the most important factor," Martin said.
Briefly passing a person on the street, at a distance of 6 feet, is likely to pose a low risk of infection, Martin said. Chatting at a distance of 6 feet with that same person for a few hours will be higher risk, he said.
Ultimately, social distancing is a powerful tool to cut all the hypothesized routes of transmission, experts said.
"If the other person is shedding virus into the air, the longer you stand near them, the greater the chance you have to be exposed to the virus," Linsey Marr, who studies the transport of air pollutants in the department of Civil and Environmental Engineering at Virginia Tech, told Live Science.
Live Science Editor-in-Chief Jeanna Bryner and Staff Writer Yasemin Saplakoglu contributed reporting to this article.
Originally published on Live Science.
OFFER: Save 45% on 'How It Works' 'All About Space' and 'All About History'!
For a limited time, you can take out a digital subscription to any of our best-selling science magazines for just $2.38 per month, or 45% off the standard price for the first three months.

Tia is the managing editor and was previously a senior writer for Live Science. Her work has appeared in Scientific American, Wired.com and other outlets. She holds a master's degree in bioengineering from the University of Washington, a graduate certificate in science writing from UC Santa Cruz and a bachelor's degree in mechanical engineering from the University of Texas at Austin. Tia was part of a team at the Milwaukee Journal Sentinel that published the Empty Cradles series on preterm births, which won multiple awards, including the 2012 Casey Medal for Meritorious Journalism.