FDA no longer requires animal testing for new drugs. Is that safe?
The FDA can now approve drugs that haven't been tested in animals, but don't expect drug companies to switch gears too quickly.

The U.S. Food and Drug Administration (FDA) no longer requires new drugs to be tested in animals before being approved. Thanks to a law passed in December 2022, the agency now has the option to approve drugs that are tested in only non-animal studies, including those that use lab-grown tissues or computer models, before being tested in clinical trials with humans.
But is that safe, and will it happen any time soon? For now, no one should expect a dramatic shift in how drug developers bring medicines to market, experts told Live Science.
"I think it's going to be a while before this actually gets implemented in full force," Vivek Gupta, an associate professor of industrial pharmacy at St. John's University told Live Science. Gupta is also the scientific founder of PulmoSIM Therapeutics, a subsidiary of VeriSIM Life that develops therapies for rare and progressive respiratory diseases.
That's because, although promising non-animal models have recently been developed, these technologies are "still in their infancy," Jim Newman, communications director at Americans for Medical Progress, which advocates for the use of animal research, wrote in a Feb. 1 statement.
Related: Why do medical researchers use mice?
Previously, the FDA typically required drugs be tested in one rodent and one nonrodent species, before they were moved into human trials, Science reported. These animal tests help reveal how drugs break down in the body, whether they reach the tissues they're intended to target and whether they exert the intended effects on those tissues — without having harmful side effects. But they're not perfect: more than 90% of drugs that pass initial animal tests end up being unsafe or ineffective in humans, according to a 2019 review in the journal Translational Medicine Communications.
Research groups developing alternatives to animal testing aim to find different models that capture this same information, or better yet, ones that accurately predict exactly how a drug will behave in people.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Dr. Donald Ingber, the founding director of the Wyss Institute for Biologically Inspired Engineering at Harvard University, agreed with Gupta's assessment that the implementation of the new law will be gradual. "It'll still be a while, I think, before we really see the impact of this," Ingber told Live Science.
One of the biggest hurdles will be convincing drug developers to adopt new, non-animal testing methods, he said. The companies will want to see evidence that the models show equivalent or superior performance to animal testing, and reassurance that the FDA views the tests as robust before they heavily invest in new technology. Once they do, that will provide the FDA with more evidence that these tests can replace animal testing.
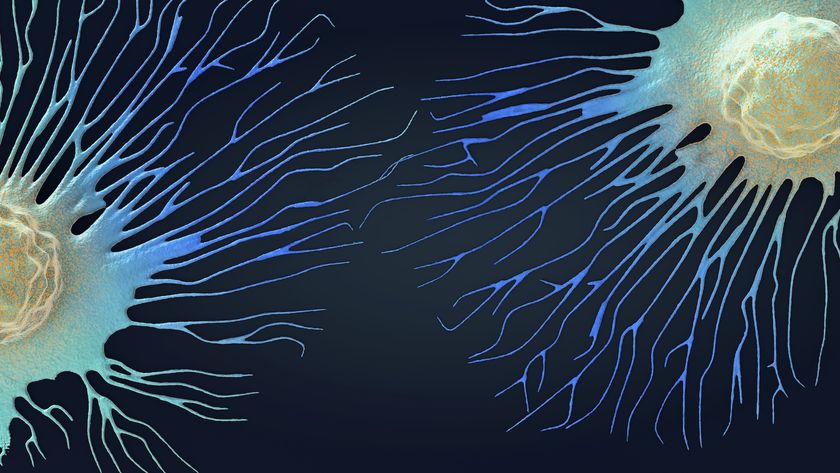
"I think it's going to happen over the next couple years, one by one, drugs including data from these models," said Ingber, whose lab develops "organ chips" — small devices that contain living human tissues and flowing fluids that mimic the inner workings of full-size organs. These organ chips, which can be used in drug testing, are being commercialized by Emulate, a biotech company of which Ingber is a board member.
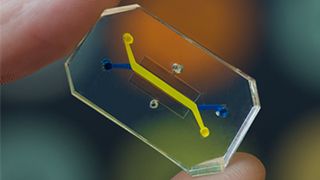
Still, replacing animal models with organ chips will "occur gradually," as each system will have to be validated for a specific purpose, to show how a drug is absorbed by the colon or whether it damages heart cells, for example, Ingber wrote in his review.
What's more, "true validation of their use as animal replacements will require large-scale evaluation involving hundreds of devices of the same design carried out using the same protocols," a feat that will require regulatory agencies and drug companies to work together to standardize their validation methods and performance criteria, he added.
Related: Tiny 'hearts' self-assemble in lab dishes and even beat like the real thing
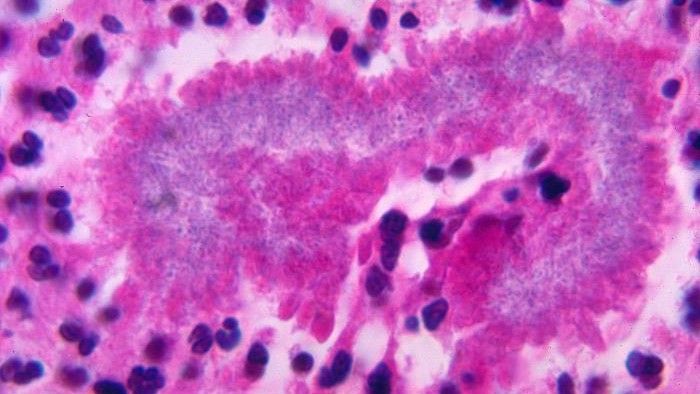
Other promising alternatives to animal testing are organoids, or 3D clusters of lab-grown cells that can mimic key biological features of full-size organs. These organized clumps, often derived from stem cells and grown on physical scaffolding, are especially useful for observing cell- and tissue-level drug responses, as well as assessing how well drugs latch onto their molecular targets, Ingber said.
"In the same ballpark" of organoids are spheroids — simpler 3D clusters of cells that are often used to model cancerous tumors, Gupta said. Gupta, who studies lung cancer, works with spheroids grown from primary cell lines, which are populations of cells sampled directly from human patients and can only replicate a few times; that's in contrast to so-called immortalized cell lines, which can be grown indefinitely.
Although often more difficult to obtain than immortal cells, primary cells better capture what happens in a human patient, Gupta explained.
Alongside these models constructed from cells are those built using computers. For instance, scientists have built computer models to assess drug toxicity — one model, described in a 2018 report in the journal Frontiers in Physiology, predicts whether a given drug could have toxic effects on the heart.
"As the AI-based models become more and more robust, as more and more data gets fed into them, I think they are able to provide a fairly accurate prediction," Gupta said. Perfecting these AI-based models will be essential in getting rid of the early stage animal tests that assess how drugs get broken down in the body and interact with different tissues, he said.
As more drug developers invest in and perfect organ chips, organoids and AI-based models the need for animal studies may gradually shrink. In the meantime, "I think the FDA will be happy to review the data," Ingber said. "If they see data that they believe are convincing, they can use it," he said.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.