85% of COVID-19 long-haulers have multiple brain-related symptoms

Many COVID-19 "long haulers" experience at least four lingering neurological symptoms, such as brain fog, headache and the loss of sense of smell or taste, even if they were never hospitalized for their initial illness, according to a new study.
For the study, published Tuesday (March 23) in the journal Annals of Clinical and Translational Neurology, the researchers analyzed information from 100 COVID-19 long haulers from 21 states. These patients were seen via telehealth or in person at the Neuro COVID-19 Clinic at Northwestern Memorial Hospital in Chicago from May to November 2020. None of the patients had been hospitalized when they initially fell ill with COVID-19-like symptoms, and all had experienced persistent symptoms for more than six weeks. On average, patients were seen four to five months after their initial illness.
Half of the participants had previously tested positive for COVID-19, while the other half had tested negative but had symptoms consistent with COVID-19. The authors note that early in the pandemic, getting a COVID-19 test was difficult for patients who didn't require hospitalization, and these patients may have cleared the infection by the time they were tested.
Related: 'We just had no answers': COVID-19 'long-haulers' still learning why they're sick
Overall, 85% of participants reported at least four neurological symptoms. The most common symptom was "brain fog" or trouble thinking, reported by 81% of participants; followed by headaches, reported by 68%; and numbness or tingling, reported by 60% of participants. More than half reported problems with their sense of taste or smell; 47% reported dizziness; 30% reported blurred vision; and 29% reported ringing in the ears.
Other common, but not neurological, symptoms included fatigue, depression and anxiety, insomnia and gastrointestinal symptoms.
In many patients, their symptoms fluctuated, or came and went, for months. When they were asked how much they felt they had recovered to their pre-COVID-19 level, on average, patients said they felt only 64% recovered after about five months.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
"Our study indicates that 'long COVID-19' is an important emerging entity requiring multidisciplinary expertise and care," the authors wrote in their paper. It's unclear how many people have long COVID, but some studies suggest that about 30% of people with COVID-19 experience lingering symptoms up to nine months after their diagnosis, Live Science previously reported.
"Although we don't know the exact number of people who are affected by long COVID,
probably millions of people in the U.S. are affected by this syndrome, and this is impacting their quality of life and cognitive function," study senior author Dr. Igor Koralnik, chief of Neuro-infectious Diseases and Global Neurology at Northwestern Medicine, said in a news conference.
More studies are needed to determine the causes of long COVID-19 and to help researchers find appropriate treatments for the condition, the authors said.
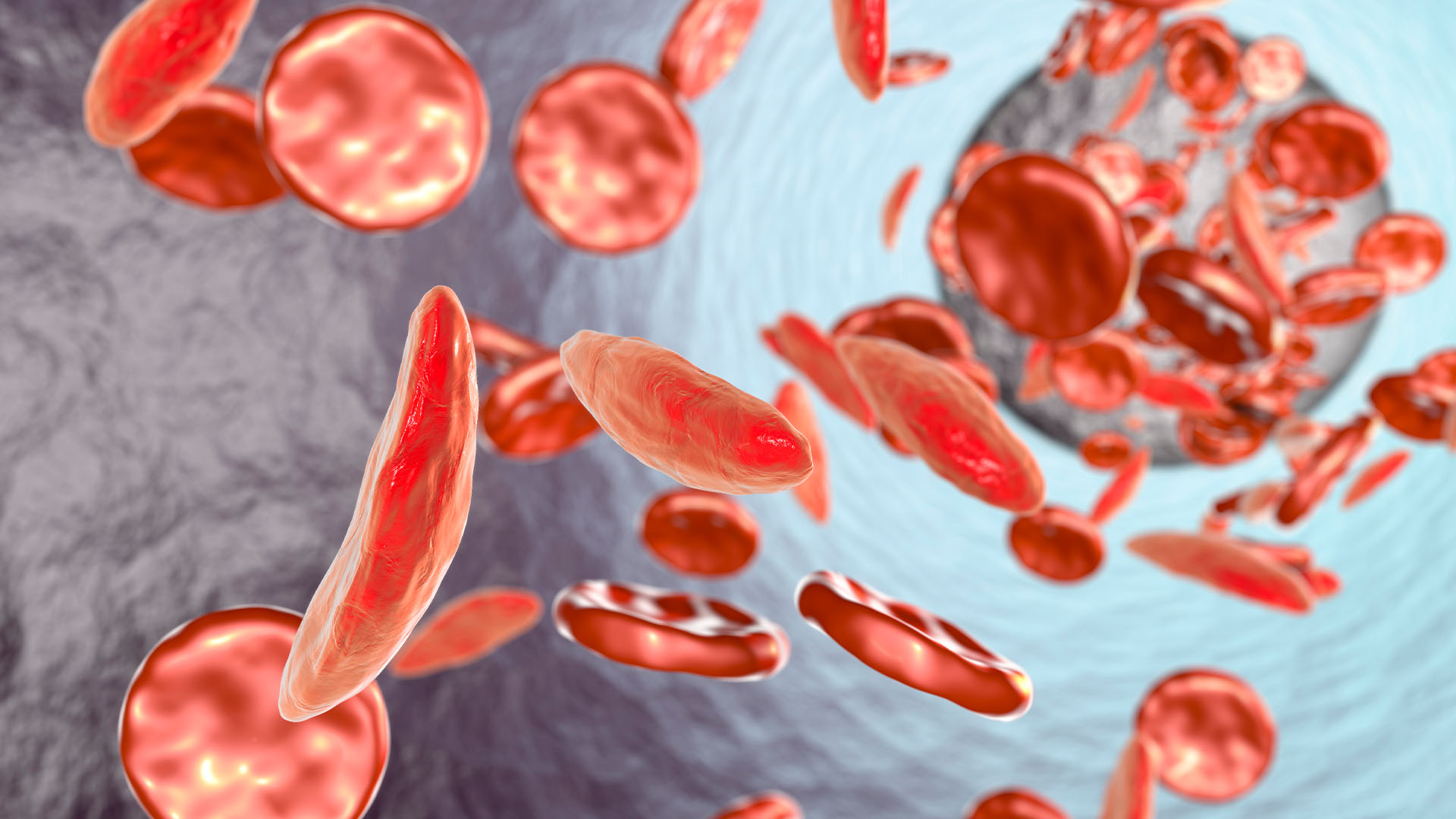
Interestingly, more than 40% of participants reported experiencing depression and anxiety prior to their COVID-19 diagnosis, suggesting this may be a risk factor for long COVID, the authors said. What's more, 16% reported having an autoimmune disease before their COVID-19 diagnosis, which is twice as high as the prevalence of autoimmune disorders in the general population, and it suggests that an autoimmune mechanism may play a role in long COVID, they said.
About 70% of participants were women, which matches the sex ratio seen in some other autoimmune disorders, such as rheumatoid arthritis, which affects three times more women than men, the authors said.
The authors note that their study was small and the majority of patients were white, and so the finding may not apply to the general population. It's also possible that some patients who tested negative for COVID-19 were not infected with the virus. The researchers are studying ways to improve COVID-19 diagnosis for those who were previously infected; for example, they are studying how certain immune cells react to the coronavirus's proteins, which may help identify those who were previously infected.
Originally published on Live Science.
Originally published on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.