What chronic fatigue syndrome can teach us about 'long COVID'
The two conditions may have similar causes.

Brain fog. Fatigue. Sleep problems. These symptoms plague many people with "long COVID" for weeks or months after recovering from COVID-19. But these symptoms are also remarkably similar to those of another disorder that's been studied for decades: myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), which is characterized partly by unexplained fatigue.
Researchers hypothesize that the two conditions may have similar causes. They also hope that existing knowledge about ME/CFS might be able to help some long COVID patients and that the study of long COVID may spur treatments for ME/CFS and better care for patients.
"I think the tools we've applied to study ME/CFS can now easily be applied to long COVID as well. And vice versa. What we've learned on long COVID is going to benefit us in ME/CFS," Dr. Avindra Nath, clinical director of the National Institute of Neurological Disorders and Stroke, told Live Science. The flip side is that after decades of study, researchers are not certain what causes ME/CFS, Nath said. Further, there is currently no cure for the condition, although patients may seek treatments for their individual symptoms, according to the CDC. Accordingly, the most significant thing ME/CFS can teach doctors about long COVID is to "be humble," he added. "What it [ME/CFS] has taught us is that there are limits to medical knowledge and to medical practice," he said.
Related: 14 coronavirus myths busted by science
Similar symptoms
ME/CFS is an umbrella term that includes both myalgic encephalomyelitis (ME), a condition that's been reported in medical literature since the 1930s, and chronic fatigue syndrome, which is characterized by exhaustion and which the medical literature first described by that name in the 1980s, according to a 2015 report by the Institute of Medicine. Symptoms of ME/CFS include fatigue after relatively minor physical and mental activities, unrefreshing sleep, brain fog, pain in joints and muscles, and dizziness and lightheadedness when standing upright, according to the CDC.
All of the aforementioned symptoms of ME/CFS have also been reported by patients with long COVID, which is defined as symptoms that appear or continue four or more weeks after first being infected with SARS-CoV-2, the virus that causes COVID-19. Additionally, both conditions are more common in women than in men, Nath said. These similarities have led doctors to wonder whether the two conditions are one and the same. Nath gave a keynote address on the topic of ME/CFS and long COVID on Aug. 20 at The International Association for Chronic Fatigue Syndrome/ Myalgic Encephalomyelitis (IACFS/ME) Conference, which was held virtually.
Common trigger
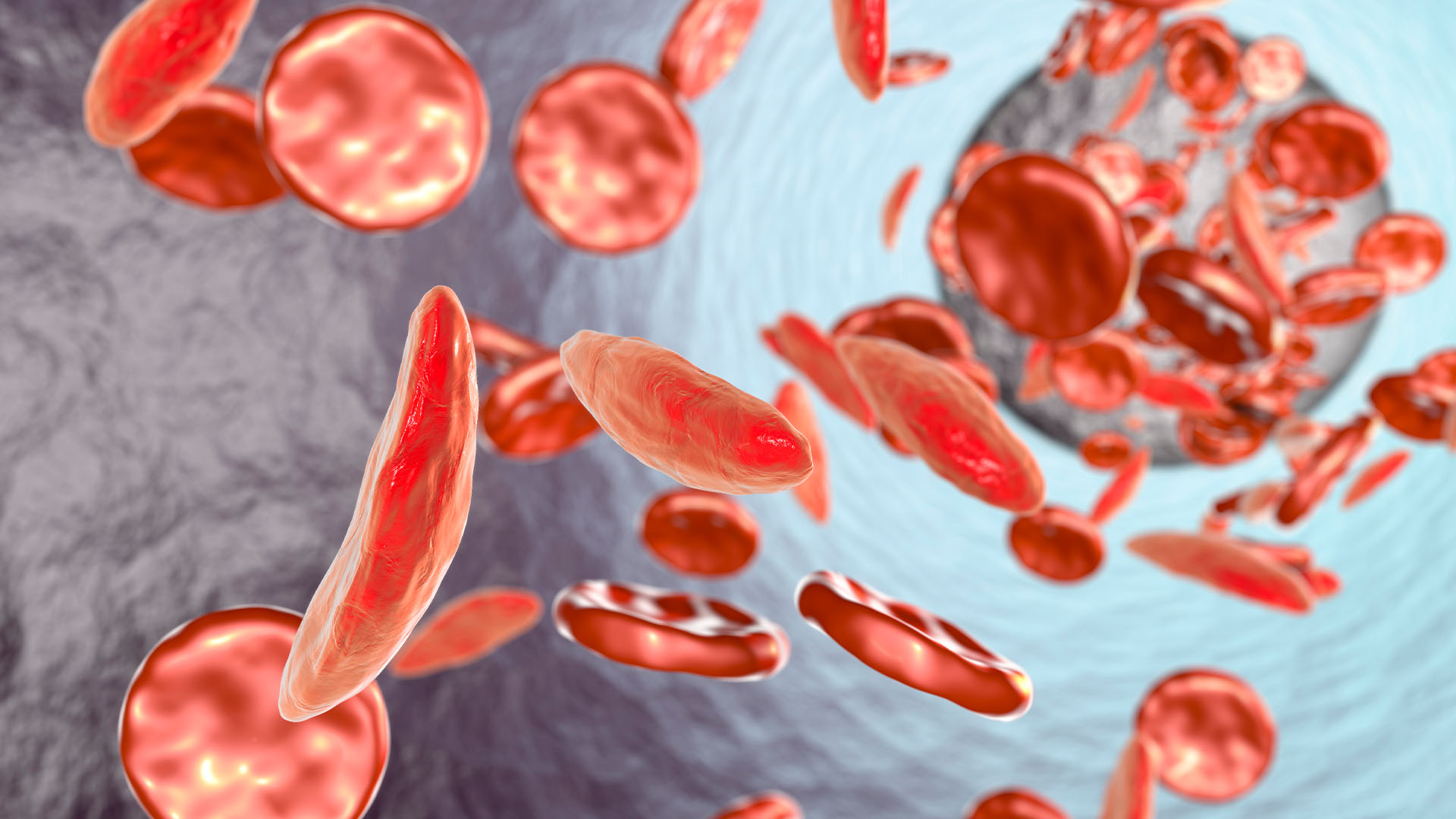
Both ME/CFS and long COVID can occur after a viral infection: Although doctors can't fully explain what causes ME/CFS, having infectious mononucleosis, or "mono," which is most commonly caused by the Epstein-Barr virus, is the most common trigger for ME/CFS, according to Leonard Jason, a psychologist who studies ME/CFS atDePaul University in Chicago. About 10% of people who are infected with Epstein-Barr virus have symptoms consistent with ME/CFS six months following the infection, according to the CDC. Not all cases of ME/CFS follow a known viral infection, however. Long-COVID, of course, follows SARS CoV-2 infection by definition.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
So one possible cause of both conditions is persistent viral infection — when a virus hides somewhere in the body where tests cannot detect it, but it can still cause trouble, Nath said. Another is that the immune system is overreacting and causing symptoms, Nath added. The immune system has two branches, adaptive (producing antibodies in response to pathogens) and innate. Nath likens the adaptive immune response, in which antibodies and T cells go after specific pathogens, to targeted missile attacks. The innate immune system, in contrast, is more like blanket bombing an entire village in hopes of killing one person within it, Nath said. The innate immune response, Nath hypothesizes, may cause symptoms of long COVID and ME/CFS. "The problem with that is once you turn on this massive, gigantic armed force, it's very hard to turn it back around again," he added.
Possible differences
Some long COVID patients, or "long haulers," as they are also known, experience an improvement in their symptoms over time, according to a study led by Jason that was published in April in the journal Fatigue: Biomedicine, Health & Behavior. The researchers surveyed 278 COVID-19 long haulers, who had been infected with COVID approximately six months earlier, about ME/CFS symptoms that they were currently experiencing and the symptoms they experienced in the first two weeks of their illness. The study participants also answered some questions about COVID-19-specific symptoms. The researchers then compared the long haulers' responses about the two time points. The team also compared long haulers' symptoms to those reported by a group of 502 ME/CFS patients, who answered the same questions about their symptoms within the last six months.
COVID-19 patients initially had more severe symptom ratings than ME/CFS patients on some measures of sleep quality, as well as for symptoms like flu and sore throat, but by the second time point, many of their symptoms had improved and become less severe than those of ME/CFS patients. An exception to this trend was that six months post infection, COVID-19 long haulers reported dizziness upon standing that was more severe than that reported by ME/CFS patients. On the other hand, the long haulers' neurocognitive symptoms, such as brain fog, worsened over time, yet remained less severe than those of patients with ME/CFS.
What do these results, which were also presented at the IACFS/ME Conference, say about whether ME/CFS and long COVID are distinct or overlapping conditions? Because COVID-19 long haulers' symptoms became less severe over time, Jason predicts that many long haulers will recover, either fully or for the most part, but that patients who are still sick after a year or two "will be very comparable, probably, to the ME/CFS case definition," he said.
While Jason predicts that long COVID patients who ultimately have ME/CFS will be a subset of the total long hauler population, Nath, on the other hand, sees essentially all cases of long COVID as being similar to ME/CFS. "Anywhere from 10 to 30% of individuals at six months post [SARS CoV-2] infection are still complaining of symptoms that could overlap with ME/CFS. Whether they are exactly the same, we still do not know, but they certainly look similar in many ways," Nath told Live Science.
Jason and Nath agree that with long COVID, many more people in the world will have a chronic-fatigue-like condition. So far in the U.S., more than 37 million people have been infected with COVID-19, according to the CDC. Even taking into account the more than 600,000 people who have died, if 10% of people infected developed long COVID (that's the lowest estimate of long COVID's prevalence) and everyone with long COVID had symptoms similar to ME/CFS, there would be at least 3.7 million cases of a condition that resembles ME/CFS.
Increased awareness
"Having more people get sick [with ME/CFS symptoms] is a tragedy, certainly. But on the other hand, it will kind of get more policy people and people within legislatures like Congress to think about the needs of these individuals," Jason said.
Most medical schools do not teach students about ME/CFS. "The illness is often misunderstood and might not be taken seriously by some healthcare providers," the CDC states. Many physicians dismiss the symptoms of patients with ME/CFS if they can't find an obvious biological cause that explains them, Jason said. People who have long COVID are facing the same sorts of problems. "I can't tell you how many people have called me with long COVID and have said, if doctors can't identify some specific organic damage to them, people are dismissing their symptoms," he said. The emergence of long COVID could prompt physicians to take ME/CSF more seriously.
Common treatment
Although there is no cure for ME/CFS, it's possible to treat — or at least attempt to lessen — some of the condition's individual symptoms, according to the CDC. For example, a person who has trouble sleeping could try over-the-counter sleep medications, talk with a doctor about prescription sleep medications, or see a sleep specialist, the CDC states, while admitting that with regard to sleep problems, "for people with ME/CFS, not all symptoms may go away." Still, the strategy of treating individual symptoms could also help people with long COVID, Jason said. "When you have people who are ill like this, they need a multidisciplinary approach to rehabilitation," he said. That can mean seeing a nutritionist, a pain specialist, a sleep specialist, or whatever health professionals treat the symptoms a patient is having, he said.
It's essential that health professionals treating ME/CFS and long COVID patients understand that what might help most people gain more energy, such as working out 30 minutes several times a week, could actually hurt these patients, Jason said. Instead, "physical and occupational therapists can help these patients with learning how to pace, learning how to structure your life in a way that doesn't make you sick," Jason said.
Originally published on Live Science.

Ashley P. Taylor is a writer based in Brooklyn, New York. As a science writer, she focuses on molecular biology and health, though she enjoys learning about experiments of all kinds. Ashley's work has appeared in Live Science, The New York Times blogs, The Scientist, Yale Medicine and PopularMechanics.com. Ashley studied biology at Oberlin College, worked in several labs and earned a master's degree in science journalism from New York University's Science, Health and Environmental Reporting Program.