How does the new coronavirus compare with the flu?
Research so far indicates that COVID-19 spreads more easily and has a higher death rate than the flu.
Editor's note: This article was updated on May 14 with the latest information on COVID-19.
Since the new coronavirus was first discovered in January, many people have compared it with a more well-known disease: The flu.
Many of these comparisons pointed to the perhaps underappreciated toll of the flu, which causes millions of illnesses and tens of thousands of deaths every year in the U.S. alone. (During the current flu season, the Centers for Disease Control and Prevention (CDC) estimates that there have been 39 million to 56 million flu illnesses and 24,000 to 62,000 flu deaths in the U.S., although that number is an estimate based on hospitalizations with flu symptoms, not based on actually counting up every person who has died of flu.)
The new coronavirus disease, COVID-19, has caused more than 1.4 million illnesses and 85,000 deaths in the U.S. as of May 14, according to data from Johns Hopkins University.
Related: Is 6 feet enough space for social distancing?
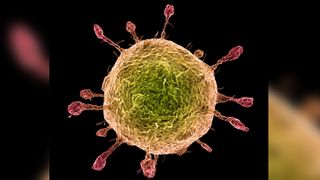
Both COVID-19 and the flu are respiratory illnesses. But COVID-19 is not the flu. Research so far indicates that COVID-19 spreads more easily and has a higher death rate than the flu.
Scientists are racing to find out more about COVID-19, and our understanding may change as new information becomes available. Based on what we know so far, here's how it compares with the flu.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Symptoms and severity
Both seasonal flu viruses (which include influenza A and influenza B viruses) and COVID-19 are contagious viruses that cause respiratory illness.
Typical flu symptoms include fever, cough, sore throat, muscle aches, headaches, runny or stuffy nose, fatigue and, sometimes, vomiting and diarrhea, according to the CDC. Flu symptoms often come on suddenly. Most people who get the flu will recover in less than two weeks. But in some people, the flu causes complications, including pneumonia. The overall hospitalization rate in the U.S. for flu this season is about 69 hospitalizations per 100,000 people, according to the CDC.
With COVID-19, doctors are still trying to understand the full picture of disease symptoms and severity. Reported symptoms in patients have varied from mild to severe, and can include fever, cough and shortness of breath, according to the CDC. Other symptoms may include fever, chills, repeated shaking with chills, muscle pain, headache, sore throat and new loss of taste or smell. COVID-19 symptoms appear to come on more gradually than those of flu, according to Healthline.
Older adults and people with underlying medical conditions, including heart disease, lung disease or diabetes, appear to be at higher risk for more serious complications from COVID-19, compared with people in younger age groups and those without underlying conditions.
The overall hospitalization rate for COVID-19 in the U.S. is about 50 hospitalizations per 100,000 people as of May 8, although the hospitalization rate for adults ages 65 and older is higher, at 162 hospitalizations per 100,000 people, according to the CDC. (However, because fewer people have likely gotten COVID-19 in the U.S. than have gotten the flu, the odds of becoming hospitalized if you have a confirmed case of COVID-19 are thought to be higher than the odds of being hospitalized with influenza.)
Children are a high risk group for complications from flu, but this doesn't seem to be the case for COVID-19 — few children have been hospitalized with the new coronavirus. A study of COVID-19 cases in the United States published March 18 found that, among 4,226 reported cases, at least 508 people (12%) were hospitalized, and of these, less than 1% were younger than 20 years old.
But recently, COVID-19 has been linked to a rare but serious inflammatory syndrome in children, called pediatric multisystem inflammatory syndrome. New York City has confirmed 100 cases of the syndrome in children, according to The New York Times.
It's important to note that, because respiratory viruses cause similar symptoms, it can be difficult to distinguish different respiratory viruses based on symptoms alone, according to the World Health Organization.
Related: Can homemade masks protect you from COVID-19?
Death rate
The death rate from seasonal flu is typically around 0.1% in the U.S., according to news reports.
Though the death rate for COVID-19 is unclear, almost all credible research suggests it is much higher than that of the seasonal flu.
It's important to note that there is no one death rate for COVID-19; the rate can vary by location, age of person infected and the presence of underlying health conditions, Live Science previously reported.
Among reported COVID-19 cases in the U.S., nearly 6% have died. This is what's known as the case fatality rate, which is determined by dividing the number of deaths by the total number of confirmed cases. But the case fatality rate is limited for a few reasons. First, not everyone with COVID-19 is being diagnosed with the disease — this is in part due to testing limitations in the U.S. and the fact that people who experience mild or moderate symptoms may not be eligible for or seek out testing. As the number of confirmed cases goes up, the fatality rate may decrease.
Researchers from Columbia University recently estimated that only 1 in 12 cases of COVID-19 in the U.S. are documented, which they said would translate to an infection fatality rate of about 0.6%, according to The Washington Post. But even this lower estimate is still at least six times higher than that of the flu. (The case fatality rate in people who become sick with flu may be 0.1%, but when you account for people who become infected with flu but never show symptoms, the death rate will be half or even a quarter of that, the Post reported.)
What's more, unlike the flu, for which there is a vaccine, everyone in the population is theoretically susceptible to COVID-19. So while the flu affects 8% of the U.S. population every year, according to the CDC, between 50% and 80% of the population could be infected with COVID-19, according to a study published March 30 in the journal The Lancet. In the U.S., that would translate to 1 million deaths from COVID-19 if half the population becomes infected and there are no social distancing measures or therapeutics, the Post reported.
Another limitation with the case fatality rate is that some people who are counted as confirmed cases may eventually die from the disease, which would lead to an increase in the death rate. For example, South Korea initially reported a case fatality rate of 0.6% in early March, but it later rose to 1.7% by the beginning of April, according to New Scientist.
Related: Why are more men dying from COVID-19?
It's also important to note that estimates of flu illnesses and deaths from the CDC are just that — estimates (which make certain assumptions) rather than raw numbers. (The CDC does not know the exact number of people who become sick with or die from the flu each year in the U.S. Rather, this number is estimated based on data collected on flu hospitalizations through surveillance in 13 states.) A recent paper published in the journal JAMA Internal Medicine emphasized this point when it found that, in the U.S., there were 20 times more deaths per week from COVID-19 than from the flu in the deadliest week of an average influenza season, Live Science previously reported.
Virus transmission
The measure scientists use to determine how easily a virus spreads is known as the "basic reproduction number," or R0 (pronounced R-nought). This is an estimate of the average number of people who catch the virus from a single infected person, Live science previously reported. The flu has an R0 value of about 1.3, according to The New York Times.
Researchers are still working to determine the R0 for COVID-19. Preliminary studies estimated an R0 value for the new coronavirus to be between 2 and 3, according to a review study published Feb. 28 in the journal JAMA. This means each infected person has spread the virus to an average of 2 to 3 people.
Some studies suggest COVID-19 has an even higher R0 value. For example, a study published April 7 in the journal Emerging Infectious Disease used mathematical modeling to calculate an R0 of nearly 6 in China.
It's important to note that R0 is not a constant number. Estimates can vary by location, depending on such factors as how often people come into contact with each other and the efforts taken to reduce viral spread, Live Science previously reported.
Pandemics
Seasonal flu, which causes outbreaks every year, should not be confused with pandemic flu, or a global outbreak of a new flu virus that is very different from the strains that typically circulate. This happened in 2009 with the swine flu pandemic, which is estimated to have infected up to 1.4 billion people and killed between 151,000 and 575,000 people worldwide, according to the CDC. There is no flu pandemic happening currently.
On March 11, the WHO officially declared the outbreak of COVID-19 a pandemic. This is the first time the WHO has declared a pandemic for a coronavirus.
Related: When will a COVID-19 vaccine be ready?
Prevention
Unlike seasonal flu, for which there is a vaccine to protect against infection, there is no vaccine for COVID-19. But researchers in the U.S. and around the world are working to develop one.
In addition, the flu has several treatments approved by the Food and Drug Administration (FDA), including antiviral drugs such as amantadine and rimantadine (Flumadine), and inhibitors of influenza, such as oseltamivir (Tamiflu) and zanamivir (Relenza). In contrast, the FDA has yet to approve any treatments for COVID-19, although approval for remdesivir, an antiviral initially developed to treat Ebola, is pending.
In general, the CDC recommends the following to prevent the spread of respiratory viruses, which include both coronaviruses and flu viruses: Wash your hands often with soap and water for at least 20 seconds; avoid touching your eyes, nose and mouth with unwashed hands; avoid close contact with people who are sick; stay home when you are sick; and clean and disinfect frequently touched objects and surfaces.
Wearing cloth face coverings in public and practicing social distancing — or staying at least 6 feet (1.8 meters) away from other people — is also recommended to prevent the spread of COVID-19.
- The 9 deadliest viruses on Earth
- 28 devastating infectious diseases
- 11 surprising facts about the respiratory system
Originally published on Live Science.
OFFER: Save 45% on 'How It Works' 'All About Space' and 'All About History'!
For a limited time, you can take out a digital subscription to any of our best-selling science magazines for just $2.38 per month, or 45% off the standard price for the first three months.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.
Most Popular


