Scientists finally have proof of mysterious immune cell in humans
These mysterious cells emerge in the womb.

While working to map every cell in the human body, scientists uncovered an elusive type of immune cell that first emerges in the womb. The existence of such cells in humans has been hotly debated — until now.
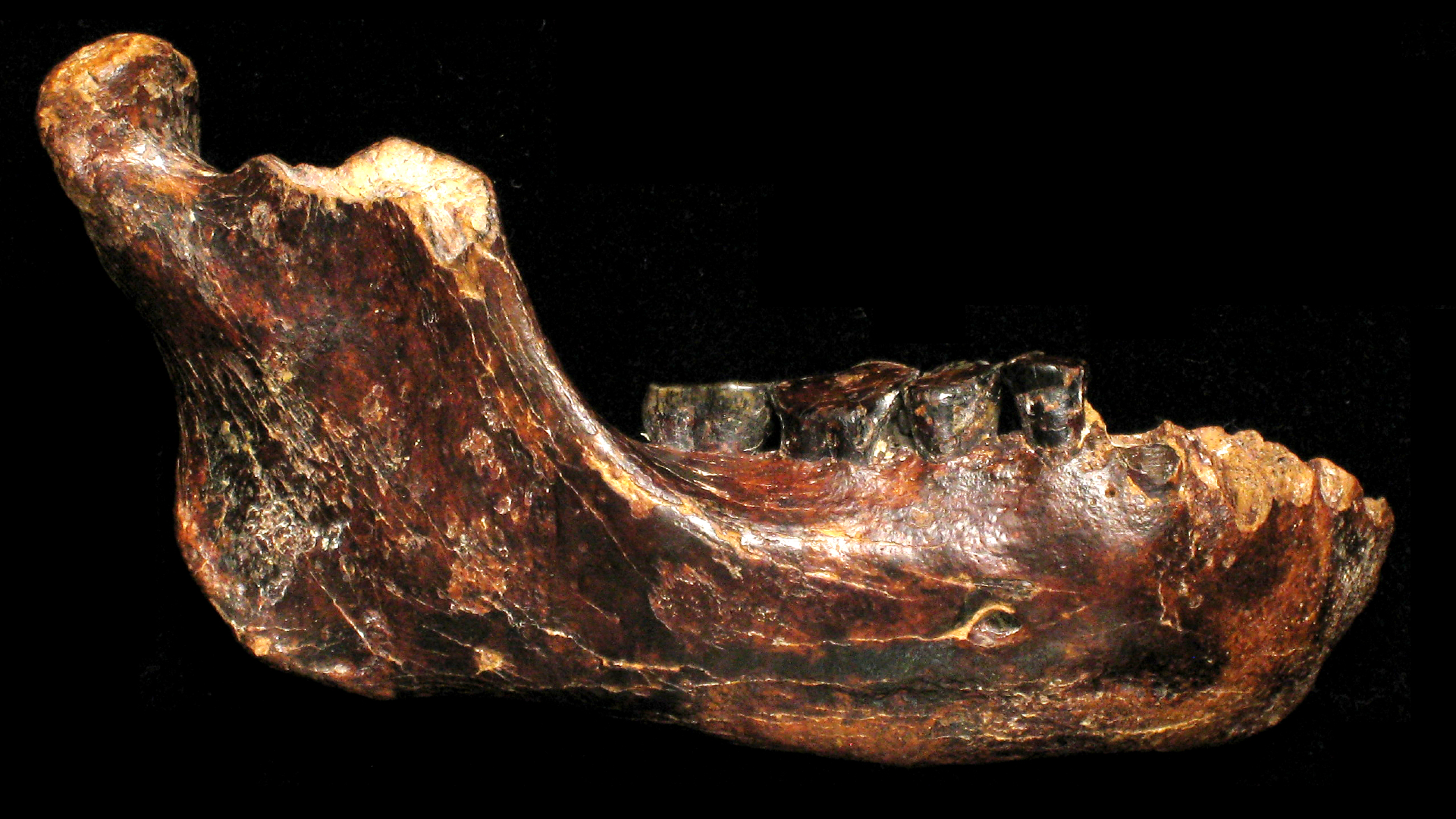
These mysterious cells, known as B-1 cells, were first discovered in mice in the 1980s, according to a 2018 review in The Journal of Immunology. These cells arise early in mouse development, in the womb, and they produce various antibodies when activated. Some of these antibodies latch onto the mouse's own cells and help to clear dying and dead cells from the body. Activated B-1 cells also make antibodies that act as a first line of defense against pathogens, like viruses and bacteria.
After the discovery of B-1 cells in mice, a research group reported in 2011 that they'd found equivalent cells in humans, but these results were not accepted as conclusive proof. "At that time, there was back and forth … Not everyone agreed with our profile of human B-1 cells," said Dr. Thomas Rothstein, a professor and founding chair of the Department of Investigative Medicine and director of the Center for Immunobiology at the Western Michigan University Homer Stryker M.D. School of Medicine, who was senior author of that previous work.
Now, a new study, published Thursday (May 12) in the journal Science, provides solid evidence that B-1 cells emerge in early human development, within the first and second trimester. "It confirms and extends the work that we published previously," Rothstein, who was not involved with the new research, told Live Science.
"I think these are the most conclusive data yet" supporting the idea that humans carry B-1 cells, said Dr. Nicole Baumgarth, a professor at the UC Davis Center for Immunology and Infectious Diseases, who was not involved in the new study. In theory, these cells may play critical roles in early development, and by studying them further, scientists can better their understanding of what healthy immune system development looks like in humans, Baumgarth told Live Science.
Related: Why do we develop lifelong immunity to some diseases, but not others?
A rare look at the developing immune system
The new research was published alongside three other studies recently conducted by the Human Cell Atlas (HCA) consortium, an international research group working to determine the position, function and characteristics of every cell type in the human body. Together, the four studies — all published May 12 in Science — include analyses of more than 1 million human cells, representing more than 500 distinct cell types sampled from more than 30 different tissues.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
"You can think of it as a 'Google Maps' of the human body, and it's really that 'street maps view' of the individual cells and where they sit in tissues that we are aiming towards," said study senior author Sarah Teichmann, head of Cellular Genetics at the Wellcome Sanger Institute in England and co-chair of the Human Cell Atlas Organizing Committee.
In helping to construct this atlas of the human body, Teichmann and her colleagues recently focused their efforts on immune cells, and in particular, the immune cells that emerge during early human development. It was through this work that they uncovered evidence of human B-1 cells. "What we show is that they do indeed exist in humans," Teichmann said during a news briefing on May 10.
The analyses featured cells from nine developing tissues, such as the thymus, a gland that makes immune cells and hormones, and the embryonic yolk sac, a small structure that nourishes the embryo in early pregnancy. All the tissue samples analyzed by the team came from the Human Developmental Biology Resource, a tissue bank in the U.K. that stores human embryonic and fetal tissues, with written permission from donors. They also incorporated publicly available data from previous HCA studies.
In all, the data covered an early period of development ranging from four to 17 weeks post-fertilization, so within the first and second trimesters.
Related: How 'Spider-Man' and 'Pac-Man' immune cells team up to fight invasive bacteria
The researchers took high-resolution snapshots of these tissues, on a 0.001 inch (50 micron) scale, which is thinner than a human hair, Teichmann said during the press briefing. And on a single-cell level, the team analyzed all the "RNA transcripts" in each tissue, which reflect the different proteins each cell makes. Using these transcripts, the researchers could make inferences about each cell's identity and function.
Through this detailed analysis, the team spotted cells that matched the description of B-1 cells found in mice, both in terms of their attributes and the timing of their emergence.
"In the mouse system, the B-1 cells arise early — they arise first," Rothstein said. A different type of immune cell, appropriately called B-2, then emerges after the first B-1 cells and ultimately becomes the most abundant form of B cell in the mouse. The new study suggests that something similar happens in humans, where B-1 cells arise and are most abundant in early development, Rothstein told Live Science.
What purpose might these special cells serve in a developing human? They may help to sculpt new tissues as they form, Teichmann said.
"When you think about fetal development, in general, there's a massive remodeling of tissues happening all the time," Baumgarth said. For example, humans initially develop webbing between their fingers, but this webbing gets trimmed back before birth. It may be that B-1 cells help direct such tissue trimming during development, but "that's speculation, on my part," she said.
In addition to sculpting tissues, the B-1 cells may provide some level of immune protection against pathogens small enough to cross the placental barrier, Baumgarth said. Again, this is speculation, she said.
The new study expands our understanding of how B-1 cells initially develop and could lay the groundwork for future studies into how the cells function later in life, Rothstein said.
Originally published on Live Science.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.