Trump is taking the latest in COVID-19 treatments. Here's how those medicines work.
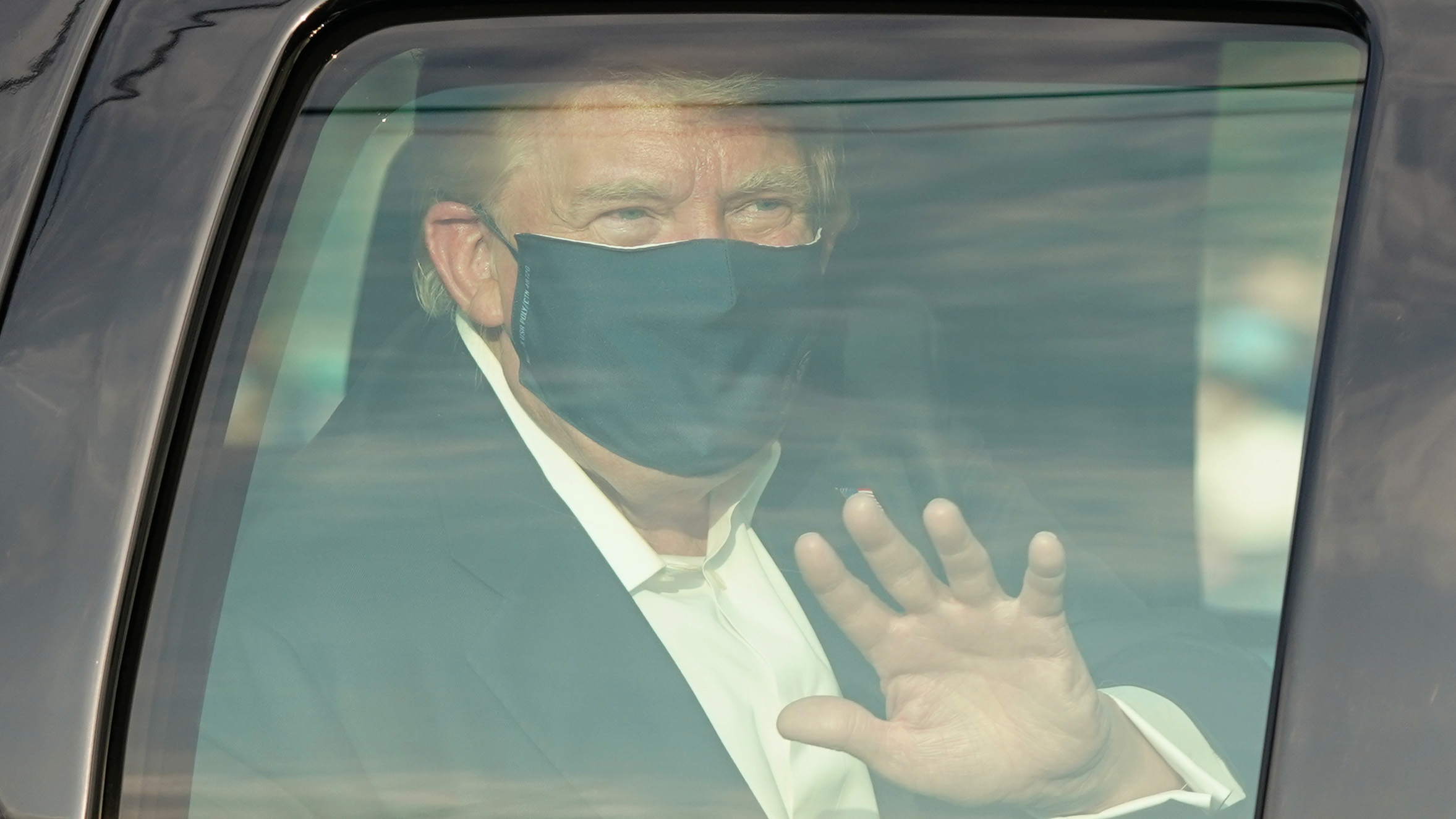
With 74-year-old President Trump and 50-year-old first lady Melania Trump testing positive for the coronavirus, what are the best proven treatments for them and other patients?
We are both physician-scientists at the University of Virginia. We care for COVID-19 patients and conduct research to find better ways to diagnose and treat COVID-19.
Here we are sharing what physicians have learned over the past eight months treating various stages of this disease. Early in the year, there were few known treatments for people who showed severe COVID-19 symptoms apart from sustaining them on ventilators. Now, several months later, there are a handful of treatments, including drugs, that give doctors far better tools to heal patients, particularly very ill ones.
Who is at greatest risk for severe COVID-19?
Men are one-and-a-half times more likely to die, and an 80-year-old has a twentyfold greater risk of death than a 50-year-old. In addition to age and male gender, obesity; diabetes; recent cancer diagnosis; chronic heart, lung and liver disease; stroke; and dementia all are associated with an increased risk of dying from COVID-19. Based on these criteria, the president falls into a higher-risk category based on male gender and age.
Is treatment different depending upon how sick one is?
The approach to therapy differs depending on the stage of the illness.
It is therefore important to not only diagnose COVID-19 but to define whether the infection is asymptomatic or pre-symptomatic. Also, how sick a person is — whether it's a mild, moderate, severe or critical case — changes how a patient is treated.
What treatment is there for asymptomatic or pre-symptomatic infection?
Asymptomatic or pre-symptomatic infection is defined as having a positive diagnostic test for COVID-19 (a PCR or antigen detection test) without symptoms of infection.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
There is currently no known effective treatment for this stage. Someone with asymptomatic or pre-symptomatic infection should isolate themself at home for 10 days so as not to expose others.
What are the symptoms of mild disease, and what treatments work?
Symptoms of mild COVID-19 infection can include fever, cough, loss of taste or smell, muscle aches, headache, nausea, vomiting, diarrhea, congestion and runny nose.
Someone with mild COVID-19 does not have shortness of breath, chest pain or evidence of pneumonia during a chest X-ray. The exception to this is children with mild disease who may still have an abnormal X-ray.
There are no treatments that have been demonstrated to benefit those with mild disease. However, such patients should be well versed on the symptoms of moderate illness, so that they and others recognize if they progress to moderate illness. This is important because progression to more severe disease can be rapid — typically five to 10 days after initial symptoms.
Moderate illness
Moderate illness is defined as shortness of breath, chest pain, or on a chest X-ray, evidence of pneumonia but without hypoxia (low blood oxygen levels).
There currently is no known effective therapy for moderate illness.
Severe illness
Severe illness is identified by a rapid breathing rate (greater than 30 breaths per minute) or low oxygen levels in the blood, which is called hypoxia. Also, evidence of pneumonia affecting more than half of the lungs, as diagnosed on a chest X-ray, is a sign of a severe case.
Controlled clinical trials have demonstrated that the antiviral drug remdesivir hastens recovery for patients with severe but not critical illness.
In addition the anti-inflammatory steroid medicine dexamethasone (a prednisonelike drug) decreases mortality.
Critical illness
Critical illness occurs when the patient becomes so sick that vital organs begin to fail and they require medicines or other therapies to support these vital functions.
If failure of the lungs is severe enough, physicians may put the patient on a mechanical ventilator or high quantities of oxygen. There is no evidence that remdesivir treatment is beneficial during this critical phase. Dexamethasone is still recommended for treatment because it has been shown to decrease mortality.
What therapies don't work or are still being tested?
Some treatments that have been shown to be ineffective include chloroquine and hydroxychloroquine.
Other potential treatments are still in the middle of clinical trials to test whether they are effective. These include human convalescent plasma, which contains antibodies that should bind to the virus and prevent it from entering cells.
There are also drugs to modulate the immune response, such as interferons and inhibitors of IL-6, which in some cases may prevent a harmful overreaction of the immune system, commonly referred to as cytokine storm.
Newer treatments, including one President Trump has been given
Right now there is no approved treatment for outpatients with asymptomatic or mild to moderate COVID-19. But this appears to be changing, with Eli Lilly's and Regeneron's release of clinical trial data on the use of laboratory-manufactured antibodies against the spike glycoprotein of the new coronavirus.
In this approach, as with convalescent plasma, the antibodies work by binding to the virus and blocking it from entering cells and multiplying. This could be particularly effective early on in infection before illness becomes severe.
[Deep knowledge, daily. Sign up for The Conversation's newsletter.]
In an early preview of data from an ongoing phase three clinical trial, subjects with COVID-19 who received an injection of a cocktail of monoclonal antibodies against the SARS-CoV-2 spike glycoprotein had symptoms that lasted only seven days rather than 13. The amount of virus remaining in the nasopharynx — the upper part of the throat behind the nose — was also reduced.
An update from the president's physician in the afternoon of October 2 indicated that, as a precautionary measure, the president received an infusion of Regeneron's antibody cocktail. This approach and others like it are currently receiving high-priority testing from the National Institutes of Health to determine whether they are safe and effective.
This article was originally published at The Conversation. The publication contributed the article to Live Science's Expert Voices: Op-Ed & Insights.
Bill Petri received his M.D. and Ph.D. (Microbiology) degrees from the University of Virginia, after which he completed his medicine residency at Case Western and then returned to UVA for an infectious diseases fellowship. He studies immunology and molecular pathogenesis of enteric infections and their consequences. Bill has served as President of the American Society of Tropical Medicine and Hygiene and Editor of Infection and Immunity, and he is currently Associate Editor for the scientific journals PLoS Pathogens, Clinical Infections Diseases and Trends in Molecular Medicine. He has received the following awards: Oswald Avery Award of the Infectious Diseases Society of America, the Burroughs Wellcome New Investigator and Scholar Awards in Molecular Parasitology, and the Lucille P. Markey Scholar Award in Biomedical Research. Since 1993, he has served on advisory committees for the National Institutes of Health (NIH).