Prostate cancer treatments can be avoided or delayed in many cases, huge study finds
A decades-long study finds that many prostate cancer patients can delay aggressive treatments and instead receive "active surveillance."

Many men with prostate cancer can delay or skip harsh treatments, such as surgery or radiation, without undermining their chances of survival, a decades-long study finds.
Instead, they can have their cancer "actively monitored" following diagnosis, rather than having their prostate removed or exposed to high-energy radiation. Such treatments can cause long-lasting side effects, such as urinary leakage, erectile dysfunction and other problems with urinary, bowel and sexual function.
"The good news is that if you're diagnosed with prostate cancer, don't panic, and take your time to make a decision" about how to proceed, lead study author Dr. Freddie Hamdy, professor of surgery and urology at the University of Oxford, told CNN. Crucially, this advice only extends to people with low- or intermediate-risk prostate cancer — those with high-risk cancer still need prompt and aggressive treatment, he said.
The new study, published Saturday (March 11) in the New England Journal of Medicine, included more than 1,600 men in the U.K. who'd been diagnosed with prostate cancer and ranged from 50 to 69 years old at the start of the trial. These patients were randomly divided into three groups that received different cancer treatments: one-third had their prostates removed, one-third got radiation in combination with a short-term hormone blocking treatment, and one-third underwent active monitoring, now commonly called "active surveillance."
Related: Dormant cancer cells may 'reawaken' due to change in this key protein
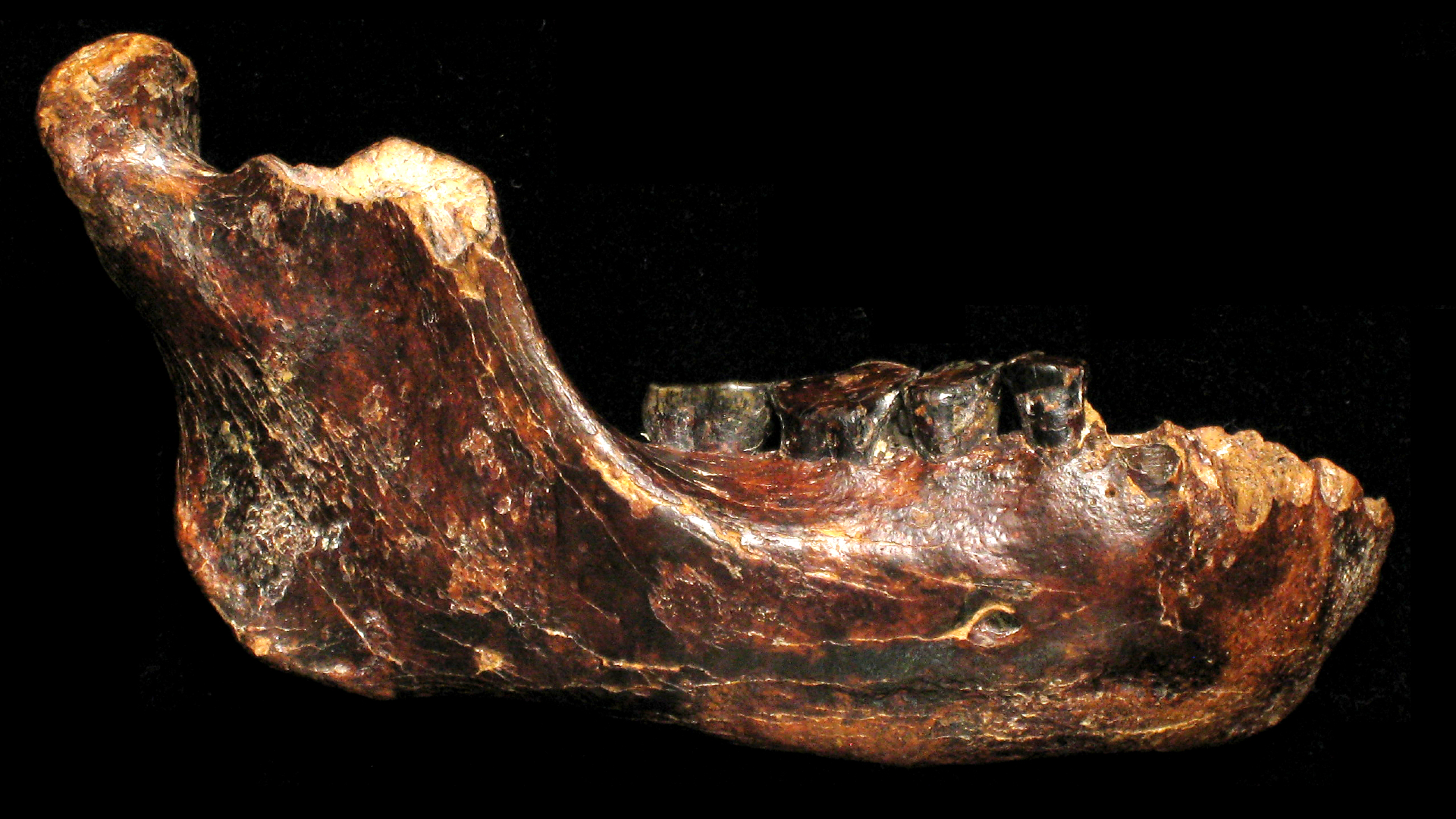
During the study, which began in 1999, active surveillance meant regularly measuring levels of a specific protein in the patients' blood. Levels of this protein, called prostate-specific antigen (PSA), tend to rise as prostate cancer progresses. Today, active surveillance can involve additional tests, such as magnetic resonance imaging (MRI) scans of the prostate and genetic testing, Dr. Oliver Sartor, medical director of the Tulane Cancer Center, wrote in a commentary of the research.
The researchers monitored each participant for 11 to 21 years post-diagnosis, and found that all the patients had a similarly low risk of death, regardless of the treatment they'd received. Overall, 45 participants, or 2.7%, died of prostate cancer. This included 12 people (2.2%) in the surgery group; 16 people (2.9%) in the radiation group; and 17 people (3.1%) in the active-monitoring group; these small differences are not considered statistically significant.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
During the roughly 15-year follow-up period, about 330 men in the monitoring group, or 60%, eventually had either surgery or radiation treatment. But waiting to get treatment didn't seem to impact their risk of death. Furthermore, 133 people in the monitoring group never had surgery, radiation or hormone blocking therapy and still survived.
At 15 years post-diagnosis, cancer had metastasized, or spread, in 9.4% of the active-monitoring group, 4.7% of the surgery group and 5% of the radiation group. However, the monitoring group may have fared better if the study had been conducted with today's methods of surveillance, Dr. Stacy Loeb, a prostate cancer specialist at NYU Langone Health who was not involved in the research, told The Associated Press. "We have more ways now to help catch that the disease is progressing before it spreads," Loeb said.
It's key to note that "the vast majority of the trial patients were at low risk or favorable intermediate risk and would today be considered appropriate candidates for active surveillance," and only a small fraction of study participants would be considered high-risk and in need of immediate treatment, Sartor wrote in his commentary.
In general, high-risk prostate cancer diagnoses account for only 15% of cases — so most of the time, prostate cancer is of low- to intermediate-risk, CNN reported. For low-risk patients, the potential risks and benefits of surgery and radiation should be carefully weighed, since "more aggressive therapy can result in more harm than good," the study authors concluded.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.
Science news this week: Controversy around the dire wolf 'de-extinctions' and a 3D hologram breakthrough
Scientists built largest brain 'connectome' to date by having a lab mouse watch 'The Matrix' and 'Star Wars'
Archaeologists may have discovered the birthplace of Alexander the Great's grandmother