'Shredder' enzyme might tear cells apart in severe COVID-19

An enzyme that can tear cell membranes to shreds may contribute to the organ damage that ultimately kills some people with severe COVID-19, a new study hints.
The enzyme, called "secreted phospholipase A2 Group IIA" (sPLA2-IIA), normally protects the body from invaders, such as bacteria, by grabbing hold of specific fats in the microbes' membranes and tearing them apart, said senior author Floyd Chilton, a biochemist and director of the Precision Nutrition and Wellness Initiative at the University of Arizona. Human cells also contain these fats, but unlike bacteria, human cells carry these fat molecules on the inner lining of their cell membranes, rather than on the outer surface.
This arrangement usually hides the molecules from sPLA2-IIA and prevents the enzyme from attacking human cells, but it's not a fool-proof system, Chilton said.
Related: 20 of the worst epidemics and pandemics in history
Cells need energy to maintain the structure of their cell membranes, but when cells begin to die due to infection or stress, the fatty molecules that sPLA2-IIA targets can become exposed, leaving human cells vulnerable to attack. In addition, damaged cells release their mitochondria, the so-called powerhouse of the cell; mitochondria resemble bacteria in terms of their membrane structure, so sPLA2-IIA rushes in to shred the free-floating mitochondria to bits and spill their contents out into the body, Chilton said. This, in turn, can call the immune system into action and set off a wave of intense inflammation, according to a 2020 report in the journal EMBO Reports.
"Once that begins to happen, you're going down a slippery slope," Chilton told Live Science.
The new research from Chilton and his colleagues hints that this disastrous chain of events may unfold in patients with severe COVID-19 infections — although we'll need more research to know for sure. For now, the study only shows a strong correlation between sPLA2-IIA and the risk of severe illness and death from COVID-19; it cannot prove that the enzyme directly causes the observed damage, Chilton said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
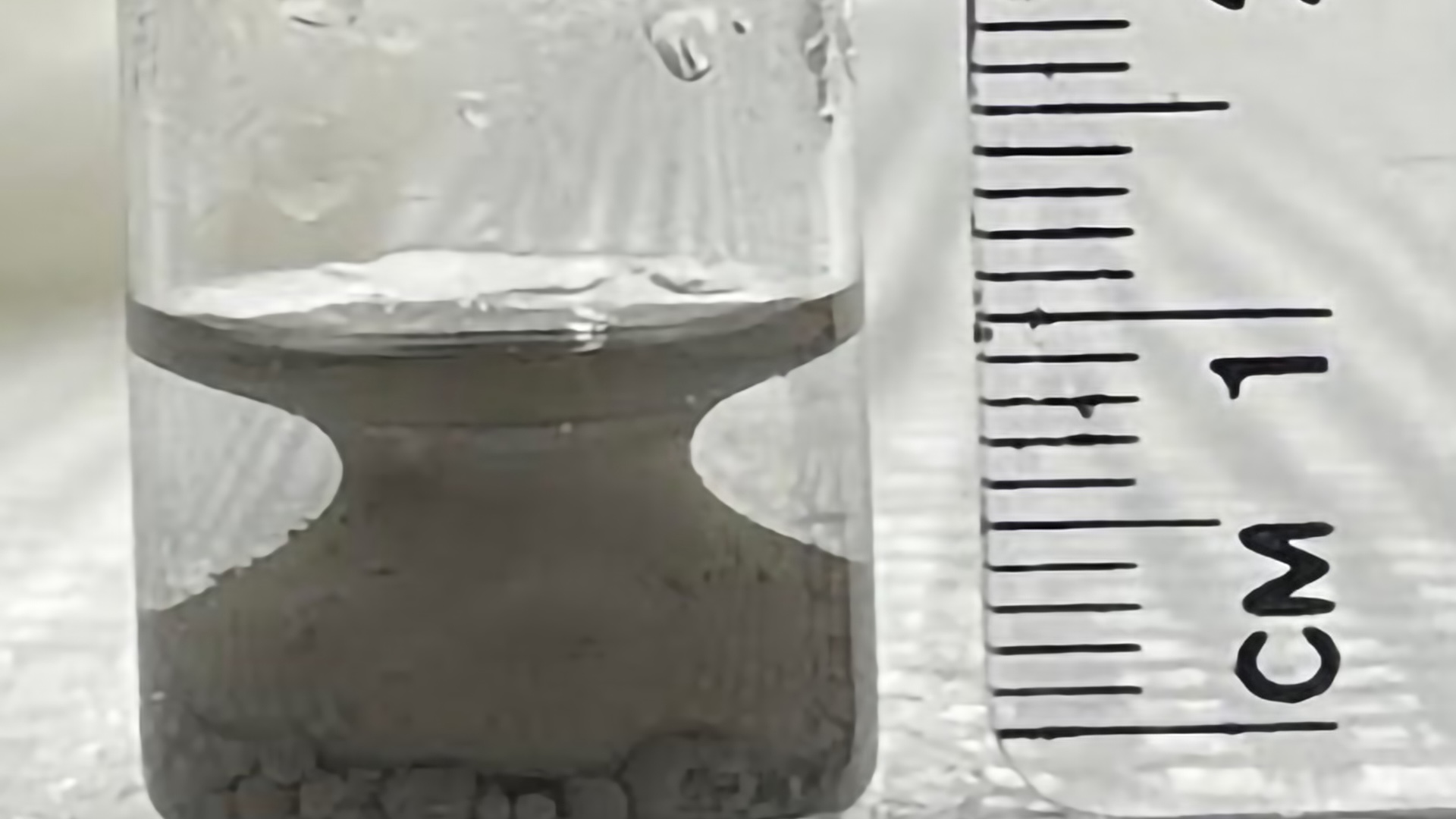
In the study, published Tuesday (Aug. 24) in the Journal of Clinical Investigation, the researchers analyzed blood samples from 127 patients who had been hospitalized between January and July 2020. Of those patients, 30 died of COVID-19; 30 experienced a severe case but survived; and 30 patients experienced mild COVID-19 infections, meaning they didn't require supplemental oxygen. The remaining 37 people did not have COVID-19 and served as a comparison group.
The team measured the levels of more than 1,000 enzymes and metabolites in the patients' blood plasma, and then used a computer algorithm to see what patterns emerged. Strikingly, they found that circulating levels of sPLA2-IIA reflected the severity of patients' disease, "particularly in deceased COVID-19 patients." In other words, a person's sPLA2-IIA levels hinted at whether or not they died from COVID-19 infection.
For context, the plasma of healthy people contains relatively low concentrations of sPLA2-IIA — at most, a few nanograms per 0.03 ounces (1 milliliter) of blood, the authors wrote in the study. "sPLA2 is normally very low, increases as the result of the viral trigger and decreases again when the inflammation resolves," Frans Kuypers, director of the Red Blood Cell Laboratory at the University of California, San Francisco, who was not involved in the study, told Live Science in an email.
Studies suggest that in severe inflammatory conditions like sepsis, sPLA2-IIA levels can skyrocket to hundreds of nanograms per milliliter. And in the new study, some of the patients who died of COVID-19 showed sPLA2-IIA levels as high as 1,020 nanograms per milliliter (ng/ml) of blood, the team reported.
Overall, the patients who died of COVID-19 had fivefold higher sPLA2-IIA levels than those who had a severe case but survived; and those who died had nearly 10-fold higher sPLA2-IIA levels than those with mild COVID-19 infections or non-COVID-related illnesses.
In addition to sPLA2-IIA, a marker of kidney function called "blood urea nitrogen" (BUN) was also linked to patients' disease severity, the team found. BUN, a waste product of protein digestion, normally gets filtered from the blood by the kidneys, but when the kidneys get damaged, BUN quickly accumulates. As COVID-19 infection damages the kidneys, high levels of sPLA2-IIA likely further damage the organ, thus raising the levels of BUN in circulation, Chilton said.
The researchers then created an index to predict the risk of COVID-19 mortality based on both BUN and sPLA2-IIA levels. They tested out the index on a group of 154 patients, separate from their original study cohort, who had been hospitalized between January and November 2020; these patients had either mild, severe or fatal COVID-19. The team found that they could predict "with reasonably high accuracy" which patients died of COVID-19 based on their sPLA2-IIA and BUN levels, and that they could also pinpoint which had severe disease but survived.
Again, the current study only identifies a correlation between sPLA2-IIA and severe COVID-19, but the results suggest that the enzyme may often be a critical factor in fatal cases, Chilton said.
"Their finding underpins the importance of this good guy [sPLA2-IIA] going bad," Kuypers told Live Science. That said, the current study has a few limitations, namely that the sample size is fairly small and the team was unable to track sPLA2-IIA levels through time, he noted. Looking forward, an ideal study would include a large number of patients whose sPLA2-IIA levels are checked daily. This would provide clearer evidence as to which patients accrue high concentrations of the enzyme, how the enzyme causes damage and whether any treatments reduce that harm, Kuypers said.
When it comes to possible treatments, drugs that work against sPLA2-IIA already exist, although none have made it all the way through clinical trials. Especially as new variants of SARS-CoV-2 emerge, it's important to identify drugs that can protect against death, regardless of which version of the virus a person catches. In this respect, targeting sPLA2-IIA may be a good idea, but we need trials to know for sure, Chilton said.
One such trial is already underway. According to ClinicalTrials.gov, investigators are currently recruiting people with severe COVID-19 for a trial of varespladib, a potent inhibitor of sPLA2 enzymes.
Originally published on Live Science.

Nicoletta Lanese is the health channel editor at Live Science and was previously a news editor and staff writer at the site. She holds a graduate certificate in science communication from UC Santa Cruz and degrees in neuroscience and dance from the University of Florida. Her work has appeared in The Scientist, Science News, the Mercury News, Mongabay and Stanford Medicine Magazine, among other outlets. Based in NYC, she also remains heavily involved in dance and performs in local choreographers' work.