10 Strangest Medical Cases of 2019
Here are 10 of the strangest case reports Live Science covered in 2019.
From a woman with purple pee to a man whose gut microbes brewed their own booze, a number of intriguing medical cases made headlines in 2019.
So-called "case reports," which describe the conditions of individual patients, don't carry the same authoritative weight as rigorous scientific studies with thousands of people participating. But such reports can sometimes help doctors better understand rare diseases or spot unusual signs of common conditions.
Here are 10 of the strangest case reports Live Science covered in 2019.
Purple pee
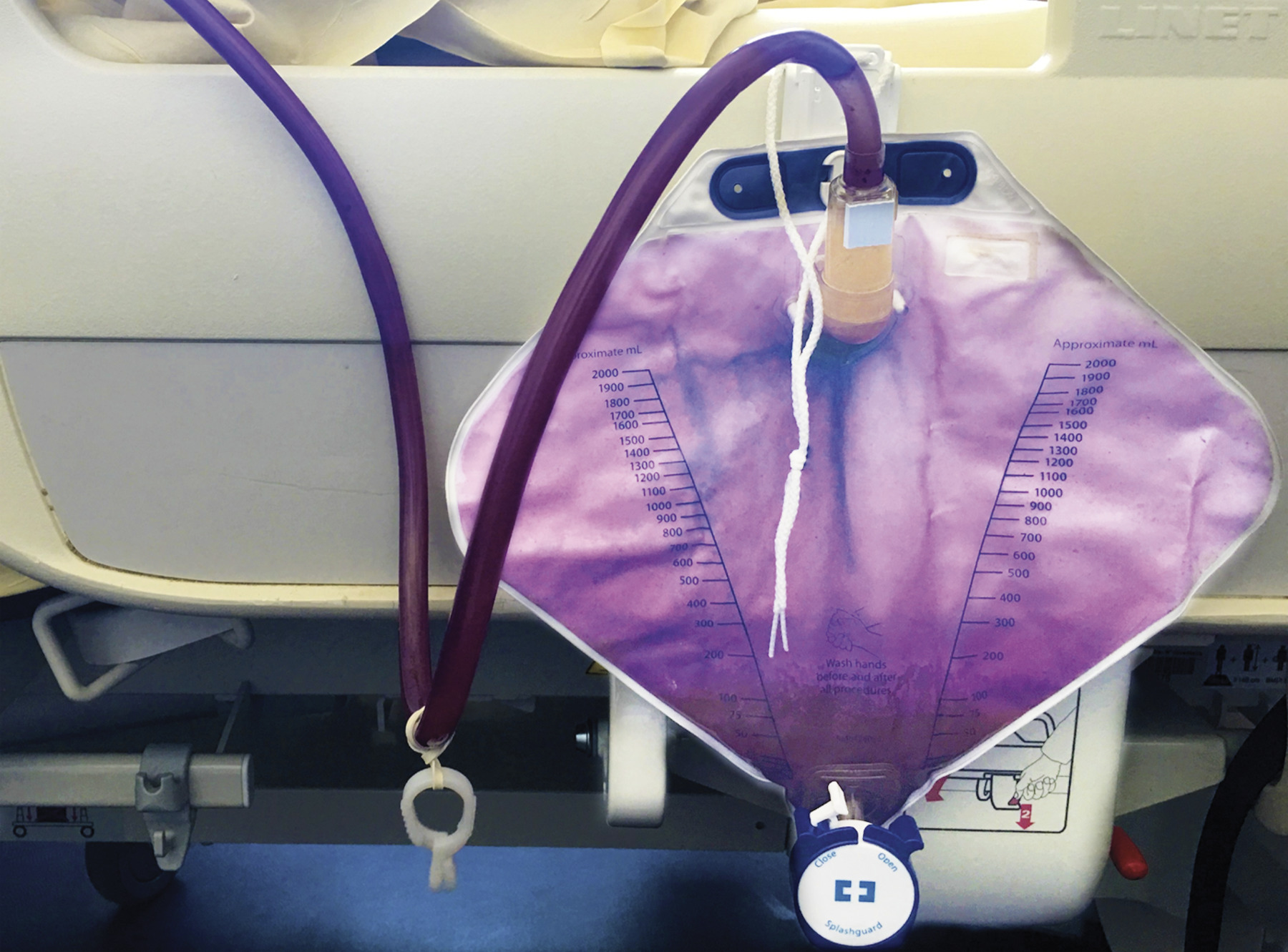
"Catheter bags," which are sometimes used to collect hospitalized patient's urine, are not usually a hot topic of discussion — unless the patient's pee turns purple. That was the case for a woman in France who, after 10 days of hospitalization, saw the pee in her catheter bag change from a normal yellow to a curious violet.
The rare condition, known simply as "purple urine bag syndrome," is the result of an odd chemical reaction that can take place inside catheter bags. It occurs when bacteria convert a chemical in urine called indoxyl sulfate — a breakdown product of the dietary component tryptophan — into red- and blue-colored compounds, which together appear purple.
Although strange-looking, purple pee itself is benign. But it can signal a urinary tract infection. Fortunately, the French woman did not have a urinary tract infection, and her pee gradually returned to normal after a four-day period of increased hydration, according to a report of the case, published Oct. 31 in The New England Journal of Medicine.
Blue blood

When a young woman in Rhode Island told doctors she was "blue," she meant it literally. The 25-year-old went to the emergency room with weakness, fatigue, shortness of breath and a bluish discoloration to her skin. When doctors drew blood from the patient's arteries, it appeared dark blue instead of the normal bright red.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
She was diagnosed with methemoglobinemia, a blood disorder in which hemoglobin, the protein in red blood cells that carries oxygen, is not able to effectively release oxygen to body tissues. The condition can cause bluish skin and blood.
The disorder can be inherited, or result from a reaction to medication. In the woman's case it was likely the latter — shortly before her symptoms started, she applied large amounts of a topical numbing medication for a toothache. She was treated with a medicine called methylene blue, which can quickly reverse the condition, and was well enough to go home the next morning, according to a report of her case, published Sept. 19 in The New England Journal of Medicine.
Mysterious intoxication

The man swore he never consumed alcohol, but his doctors refused to believe him — not only did the man appear drunk, his blood alcohol level was very high. But as it turns out, the man was telling the truth — he had a rare condition in which his gut microbes brewed their own booze.
For six years, the 46-year-old man experienced episodes of mysterious drunkenness, according to a report of his case, published Aug. 5 in the journal BMJ Open Gastroenterology. During these episodes, he experienced mental changes, including "brain fog," as well as uncharacteristically aggressive behavior. One day, he was arrested for drunken driving and found to have a blood alcohol level twice the legal limit. All the while, he denied consuming any alcohol.
Eventually, doctors diagnosed the man with auto-brewery syndrome (ABS), which happens when microorganisms in the gut ferment carbohydrates into alcohol. In the man's case, he had strains of yeast living in his gut that convert carbs to booze. Antibiotics wiped out these boozy microbes, and probiotics helped reestablish a healthy gut microbiome. He was eventually able to eat carbs again without becoming intoxicated.
Wasabi overload

Wasabi and avocado are both popular, green foods, but you probably don't want to confuse one with the other given their drastically different tastes and levels of spiciness. What's more, for a woman in Israel, this mixup may have led her to develop "broken-heart syndrome."
The 60-year-old woman was attending a wedding when she ate "a large amount of wasabi," which she thought was avocado, according to the report, published Sept. 20 in the journal BMJ Case Reports. A few minutes later, she felt a "sudden pressure in her chest radiating to her arms," the report said.
The next day, she was diagnosed with broken-heart syndrome, a condition in which the heart's main pumping chamber, the left ventricle, becomes enlarged and weakened so that it doesn't pump properly. The condition can be triggered by emotional or physical stress. In this case, doctors suspect that the burning mouthful of wasabi may have triggered the woman's syndrome. Fortunately, the condition is usually temporary, and the woman recovered after about a month of treatment with heart medications.
"Penile ossification"

Sometimes, the body grows bone in places it shouldn't. For one 63-year-old man, this happened in the penis.
The man underwent a pelvic X-ray after a fall, and doctors discovered there was "ossification" along the entire shaft of his penis, according to a report of the case, published in the September issue of the journal Urology Case Reports. In other words, his penis was turning to bone.
The man was diagnosed with "penile ossification." The condition is very rare, with fewer than 40 cases reported in the medical literature. Ossification happens when calcium salts build up in soft tissues, leading to bone formation.
Chest fire

When a man's chest caught fire during heart surgery, it wasn't a case of spontaneous combustion. Rather, it was a rare surgical complication that's known to occur under the right circumstances.
The 60-year-old man needed surgery to fix a life-threatening tear in his chest artery, according to the report, presented in June at a meeting of the European Society of Anaesthesiology. The man had a history of chronic lung disease, and during the surgery, doctors needed to give the man a high dose of supplemental oxygen to prevent breathing problems. Doctors also used an electrocautery device, which heats tissue with electricity, to stop blood vessels from bleeding.
Suddenly, sparks from the electrocautery device ignited a fire on the surgical gauze. The fire was quickly extinguished with saline (salt water), without injury to the patient.
The use of supplemental oxygen likely contributed to the surgical fire. Oxygen itself does not burn, but it lowers the temperature at which a fire can start. Despite the incident, the rest of the man's surgery went well, and doctors successfully repaired the tear.
"Hair splinter"

A fallen strand of hair seems harmless enough. But in rare cases, loose hair can become embedded in the skin, essentially causing a "hair splinter."
That was the case for a 35-year-old man in Brazil, who went to the emergency room with a mysterious pain in his right heel that got worse when he walked.
When doctors first looked at his foot, they couldn't see anything wrong. But a closer look at the heel revealed a single strand of hair seemingly attached to his foot. The man was diagnosed with cutaneous pili migrans, a rare condition in which a hair shaft or hair fragment becomes embedded in the skin's surface. Only about 26 cases of cutaneous pili migrans have been reported in the last 60 years.
Doctors used tweezers to remove the hair, which measured only 0.4 inches (10 millimeters). Afterward, the man immediately felt relief from the pain, according to the report, published June 20 in The Journal of Emergency Medicine.
Blinding diet

Junk food diets aren't just bad for your waistline and your heart, they can also be bad for your eyes. Indeed, a British teen who ate nothing but fries, chips and other junk food for years slowly went blind as a result of his poor diet, according to a report of the case published Sept. 2 in the journal Annals of Internal Medicine.
The teen was reportedly a "fussy eater," and at age 14, he was found to have low levels of vitamin B12. By age 15, he developed hearing loss and vision problems, and by 17, he was "legally blind" in both eyes. Tests showed the teen had developed damage to his optic nerve, the bundle of nerve fibers that connects the back of the eye to the brain.
When doctors asked what foods he ate, the patient confessed that the only things he ate were fries, chips — specifically, Pringles — white bread, processed ham slices and sausage. He was diagnosed with nutritional optic neuropathy, or damage to the optic nerve that results from nutritional deficiencies. It's known that the B vitamins are essential for many cellular reactions, and deficiencies in these vitamins can lead to the buildup of toxic byproducts, and eventually to the damage of nerve cells.
The teen's vision loss was permanent, but he was prescribed nutritional supplements, which prevented his vision from getting any worse. He was also referred to mental health services for an eating disorder.
"Collapsed" iris
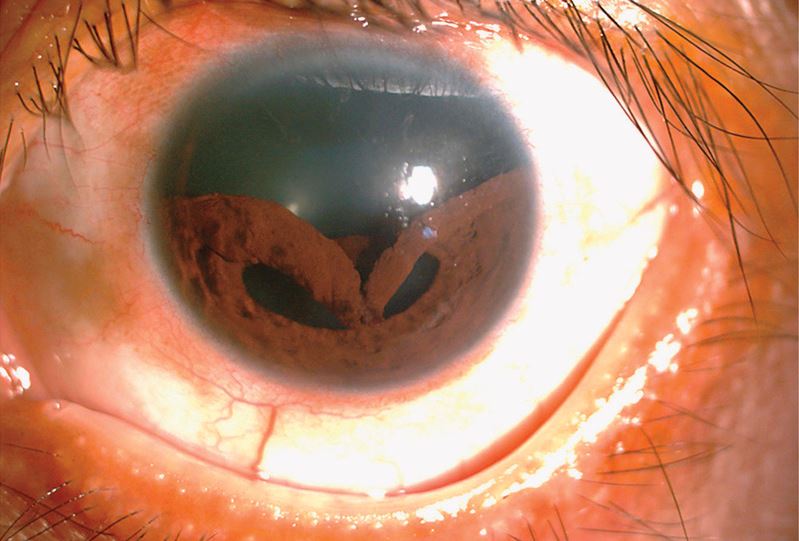
You might not think of the iris — the colored part of the eye — as something that can just "collapse." But this can happen with certain eye injuries, as was the case for a man in Taiwan when an injury caused his iris to detach from its normal place and droop downward.
The man went to an eye clinic after being struck in his left eye with a bungee cord, according to a report of the case, published April 10 in The New England Journal of Medicine. The man reported pain and double vision in his eye.
He was diagnosed with "traumatic iridodialysis," a type of eye injury that happens when blunt trauma causes the iris to detach from the circular structure behind it, known as the ciliary body. The man underwent a surgery known as "iridoplasty" to try to reposition his iris. Afterward, he his pupil shape was restored and eyesight improved.
"Milky" blood
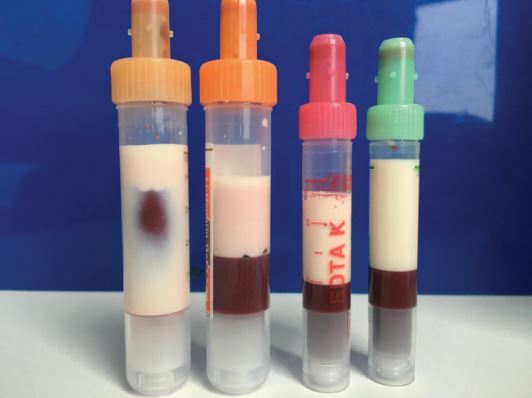
A man's blood was so thick with fat, it turned a milky color.
The 39-year-old man had diabetes, but wasn't taking his medications regularly, according to a report of the case, published Feb. 25 in the journal Annals of Internal Medicine. He went to the emergency room with nausea, vomiting, headaches and decreased alertness.
Tests revealed he had extraordinarily high levels of triglycerides, a type of fat, in his blood. Triglyceride levels below 150 milligrams per deciliter (mg/dL) are considered normal, and levels above 500 mg/dL are considered "very high." The man's triglyceride levels clocked in at more than 14,000 mg/dL.
Doctors tried using a machine to filter the fat out of the man's blood — a process known as plasmapheresis. But the machine became clogged due to the extremely high blood fat levels. So they turned to bloodletting, or the manual withdrawal of blood, to save that man's life. It appears to be the first reported cases of bloodletting to treat high levels of triglycerides, or hypertriglyceridemia, the authors said.
Originally published on Live Science.

Rachael is a Live Science contributor, and was a former channel editor and senior writer for Live Science between 2010 and 2022. She has a master's degree in journalism from New York University's Science, Health and Environmental Reporting Program. She also holds a B.S. in molecular biology and an M.S. in biology from the University of California, San Diego. Her work has appeared in Scienceline, The Washington Post and Scientific American.