How did doctors perform surgery before modern anesthesia?
Before there were medicines to sedate and soothe patients, there was opium, mandrake juice … and hypnosis.

In 1811, English novelist Fanny Burney underwent a mastectomy without so much as a shot of whiskey to dim the pain. In letters she wrote to her sister after the operation, she recalls, "I began a scream that lasted unintermittingly [sic] during the whole time of the incision — and I almost marvel that it rings not in my ears still! So excruciating was the agony." In fact, Burney fainted twice from the pain of the incision, which likely came as a welcome relief.
Her operation took place during a time when surgical anesthesia was still in its infancy, and the limited options that existed could be unreliable and often dangerous. Historical anecdotes like hers reveal "what a disgusting thing surgery was before anesthesia," said Tony Wildsmith, professor emeritus of anesthesia at the University of Dundee in Scotland, and former honorary archivist at the Royal College of Anaesthetists in the United Kingdom.
Indeed, confronting such pain would be nightmarish. Today, anesthetics are now a fixture in medicine, comprising an array of drugs that are used not just for managing pain but also for relaxing muscles and making patients unconscious. Many people will, at some point in their lives, receive these drugs — whether it's a localized anesthetic to numb their gums at the dentist's office, an epidural during childbirth or a general anesthetic to induce a deep slumber while doctors remove tonsils.
But how did doctors do surgery before anesthetics? The answer reveals a cruder, more painful and occasionally suspect history.
Related: Why do doctors wear green or blue scrubs?
Pain through the ages
Anesthesia as we know it today is a relatively new invention, but for centuries, we have been searching for ways to soothe severe pain. As far back as the 1100s, there are accounts of physicians applying sponges soaked with opium and mandrake juice to patients to induce sleepiness in preparation for an operation, and to dull the pain that followed.
Going back even further, manuscripts stretching from Roman to medieval times describe a recipe for a sedative mixture called "dwale." Made from a heady concoction of boar bile, opium, mandrake juice, hemlock and vinegar, the tincture was brewed "to make a man sleep whilst men cut him," according to one manuscript from the Middle Ages. From the 1600s onward in Europe, opium and laudanum (opium dissolved in alcohol) became common pain relievers.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
But these medicines would have been crude, inexact and difficult to tailor to patients and their needs. What's more, they could be dangerous; hemlock can be fatal, for instance, and opium and laudanum are addictive. Mandrake in high doses can cause hallucinations, abnormal heart rate — and in extreme cases, death.
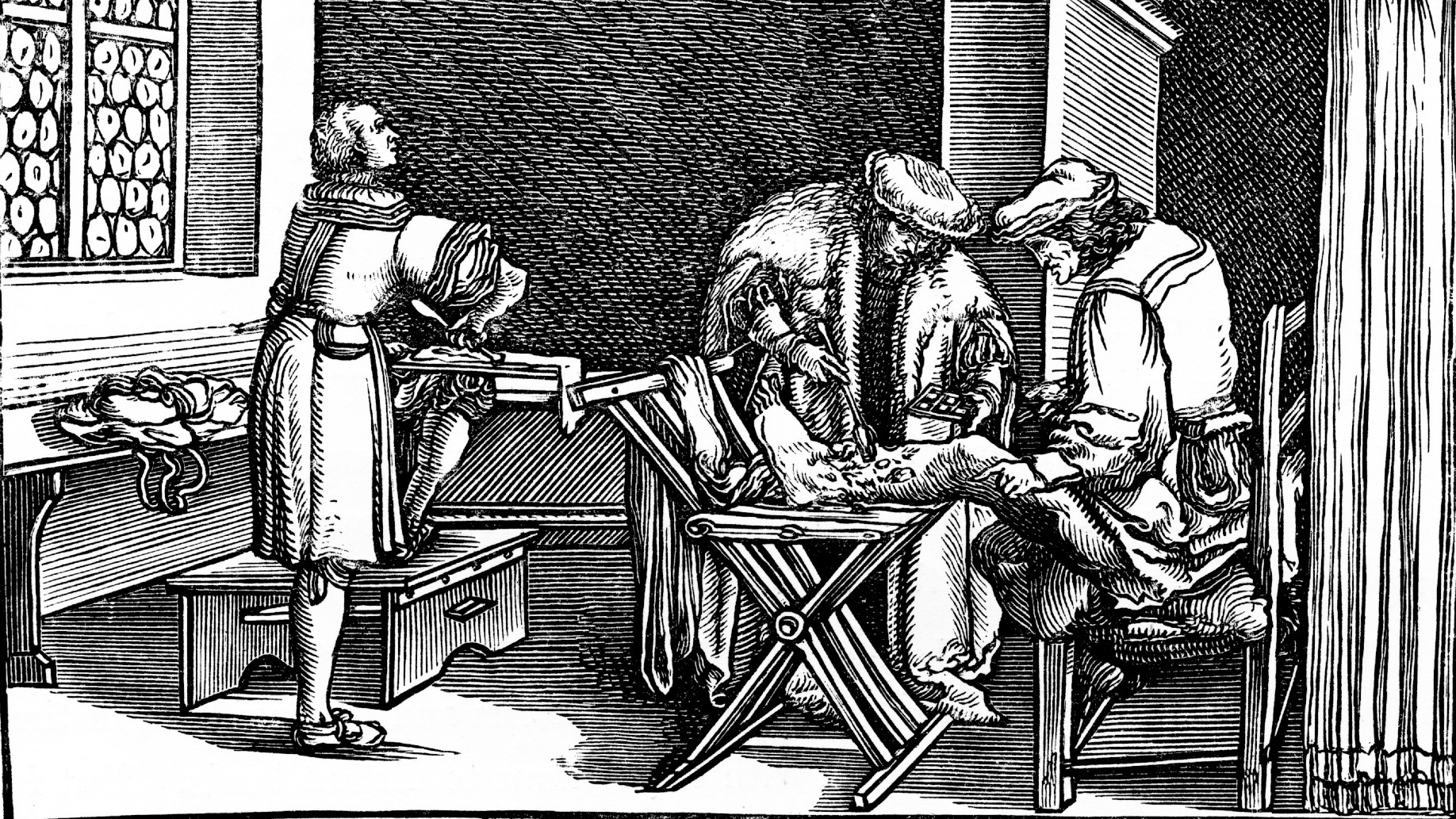
Against the backdrop of this unforgiving medicinal landscape, when surgeons did have to perform invasive surgeries, often the most sensible method they employed was simply to be as quick and precise as possible. "You go back 150-plus years, and surgery was brief," Wildsmith told Live Science. Efficiency and precision under time pressure became a measure of a surgeon's skill.
But speed and precision also confined surgeons to less-complex operations. For example, it's safe to assume that before the advent of surgical anesthesia in Europe and the United States in the mid-1800s, high-stakes surgeries such as cesarean sections and amputations in these regions would have been less common than they are today, both because of the skill and risks involved and the intense and unmanageable pain they would bring about, Wildsmith told Live Science. "There weren't many operations described, because there wasn't the ability to do them," he said.
In fact, dentistry was one of the few types of surgery that was comparatively more common during this period, because the pain and dangers involved in doing it were lower than in more serious types of surgery, Wildsmith explained. Needless to say, patients weren't exactly lining up to have these operations, either. "Try and put yourself in that position," Wildsmith said. "You've got pain, but the pain of having it relieved would be even worse."
Related: Why is the medical symbol a snake on a stick?
Questionable methods
As surgeons sought new ways to do their work, some more unusual methods came about. One of these was compression, a technique that involved applying pressure to the arteries to render someone unconscious, or to the nerves to cause sudden numbness in the limbs.
The first technique possibly stretches back to ancient Greece, where physicians named the arteries in the neck the "carotids," a word with a Greek root meaning "to stun" or "stupefy." "So, there's evidence that they used it or knew that compression of the carotid arteries would produce unconsciousness," Wildsmith said. He emphasized, however, that there's no suggestion that this method was widely applied — and probably with good reason. Someone trying this extremely risky method today would be "more likely to end up in the dock for a charge of murder than anything else," Wildsmith said.
In 1784, a British surgeon named John Hunter tried compression of the nerves by applying a tourniquet to a patient's limb and causing numbness. Surprisingly, it worked: Hunter was able to amputate a limb, and apparently, the patient felt no pain, according to the Royal College of Anaesthetists.
Another pain management technique was 'mesmerism.' This pseudoscientific belief combined elements of hypnosis with theories that there was a force-field-like liquid in humans that could be manipulated with magnets, the Hektoen International Journal reported. The technique's inventor, Austrian physician Franz Anton Mesmer, believed that by controlling this malleable fluid, he could put patients in a state of suspended animation, during which they would be oblivious to the pain of surgery.
These pseudoscientific practices gained real traction. By the mid-1800s, mesmerism had spread to other parts of Europe and to India, and surgeons used it to operate on patients. And, in several instances, the patients were reportedly pain-free, according to a report in the Hektoen International Journal. Mesmerism became so popular, in fact, that several "mesmeric hospitals" were established in London and elsewhere.
But surgeons began to question these methods and accuse proponents of misleading the public. A rivalry ensued, and mesmerism was discredited. This set the stage for new and more promising candidates for pain relief and sedation: a series of inhalable gases that, by the mid-1800s, were poised to launch a new era of modern anesthesia, according to the Hektoen International Journal.
From pseudoscience to modern anesthesia
Leading up to the mid-1800s, scientists and surgeons grew increasingly interested in the clinical use of a sweet-smelling organic compound called ether, made by distilling ethanol with sulfuric acid. In fact, records of ether production go back as far as the 13th century, and in the 16th century, physicians experimenting with the mysterious substance discovered it could anesthetize chickens.
Related: What did people use before toilet paper was invented?
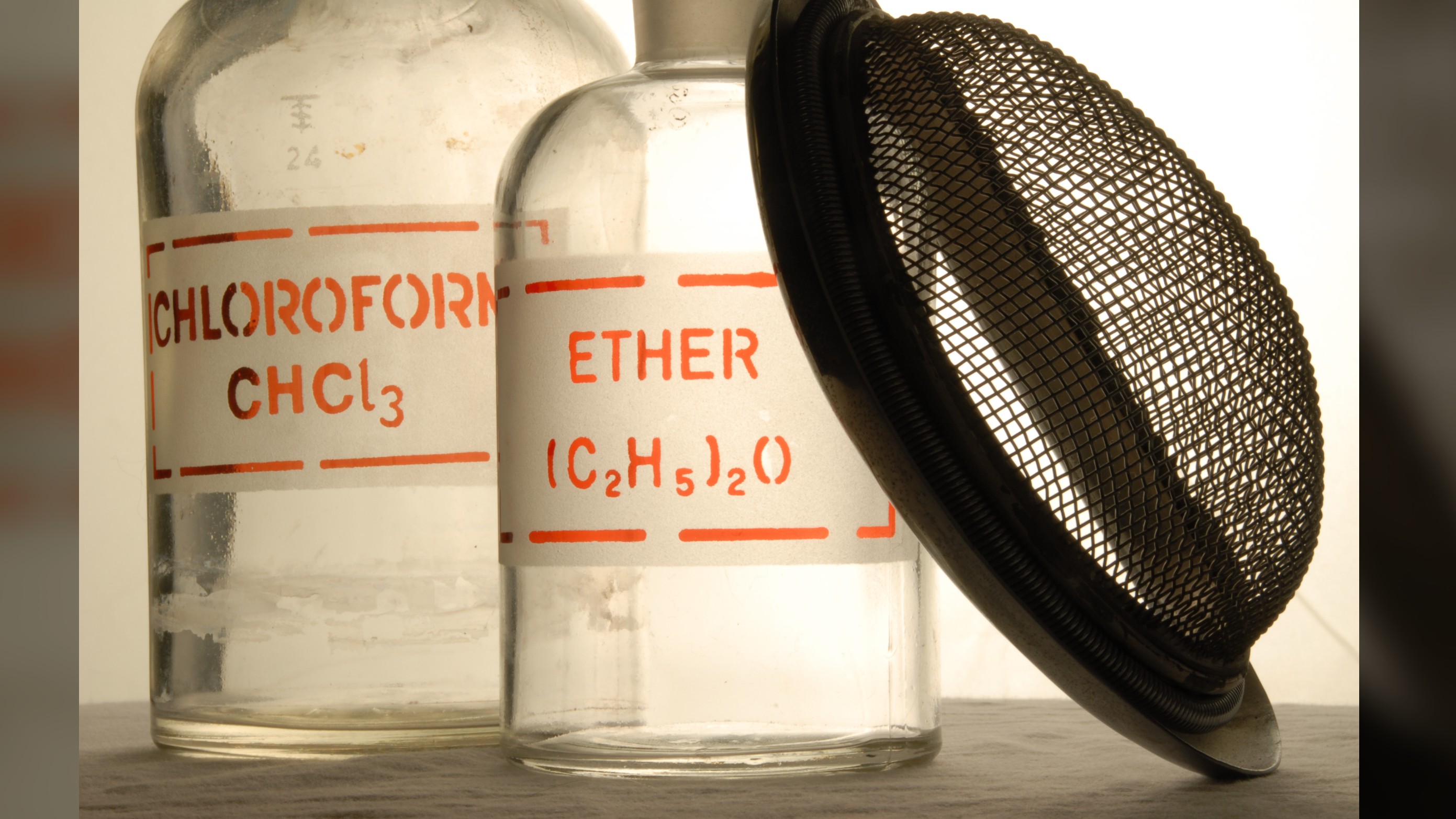
Several hundred years later, surgeons revisited ether in their work. "There were people scratching at the surface for a long time,"Wildsmith said. Finally, in 1846, an American dental surgeon named William Morton carried out a public operation in which he supplied gaseous ether to a patient and then painlessly removed a tumor from the patient's neck. It was the first clinical proof that the careful application of this gas could cause unconsciousness and ease pain.
Then, in 1848, surgeons proved that another compound, called chloroform, could successfully ease pain during childbirth and other surgeries. Critically, ether and chloroform gave surgeons more control over the condition of their patients, because by managing patient's pain and sending them to sleep, it bought surgeons more time to operate and therefore to do so more meticulously. Over time, this enabled more sophisticated surgeries. Neither of the two gases is used surgically anymore, but both ultimately laid the groundwork for the development of safer and more effective drugs that have turned anesthesia into the fine-tuned art it is today.
Wildsmith recalled an 18th-century oil painting that shows a man gaping in horror as he undergoes an amputation. "It genuinely depicts, by the look on the patient's face, what an awful exercise that must have been for a patient without anesthesia," Wildsmith said.
Anesthesia's history may be full of trial and error, but anyone who's ever set foot in a hospital can be grateful that at least it's taken us far from the nightmarish realities of that painting.
Originally published on Live Science.

Emma Bryce is a London-based freelance journalist who writes primarily about the environment, conservation and climate change. She has written for The Guardian, Wired Magazine, TED Ed, Anthropocene, China Dialogue, and Yale e360 among others, and has masters degree in science, health, and environmental reporting from New York University. Emma has been awarded reporting grants from the European Journalism Centre, and in 2016 received an International Reporting Project fellowship to attend the COP22 climate conference in Morocco.