Tuberculosis: Symptoms, Treatment & Prevention
Reference Article: Facts about tuberculosis.
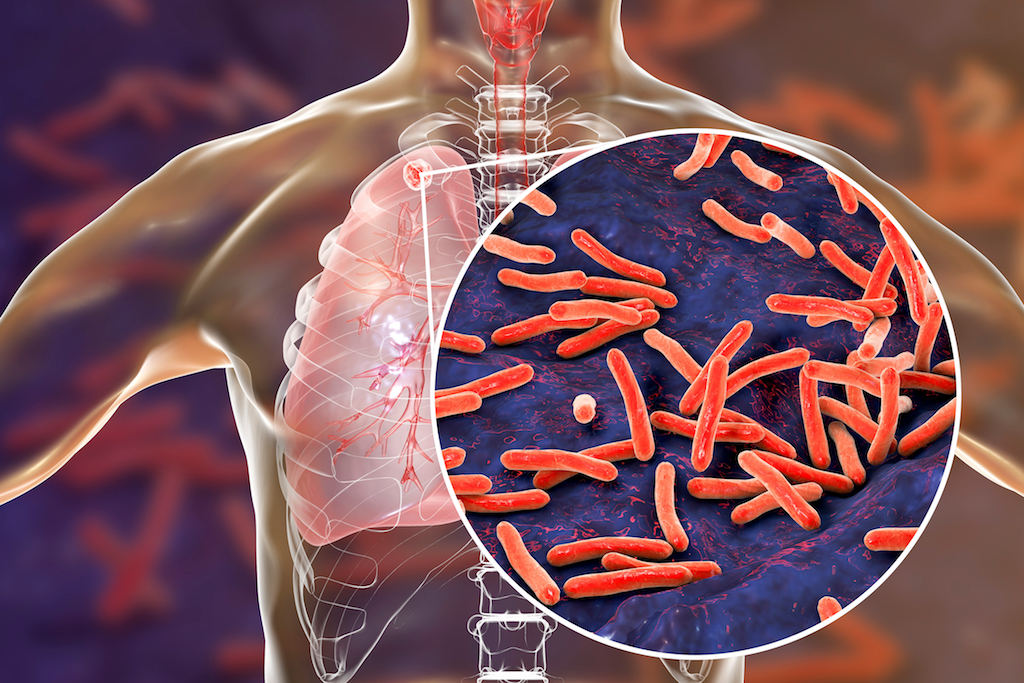
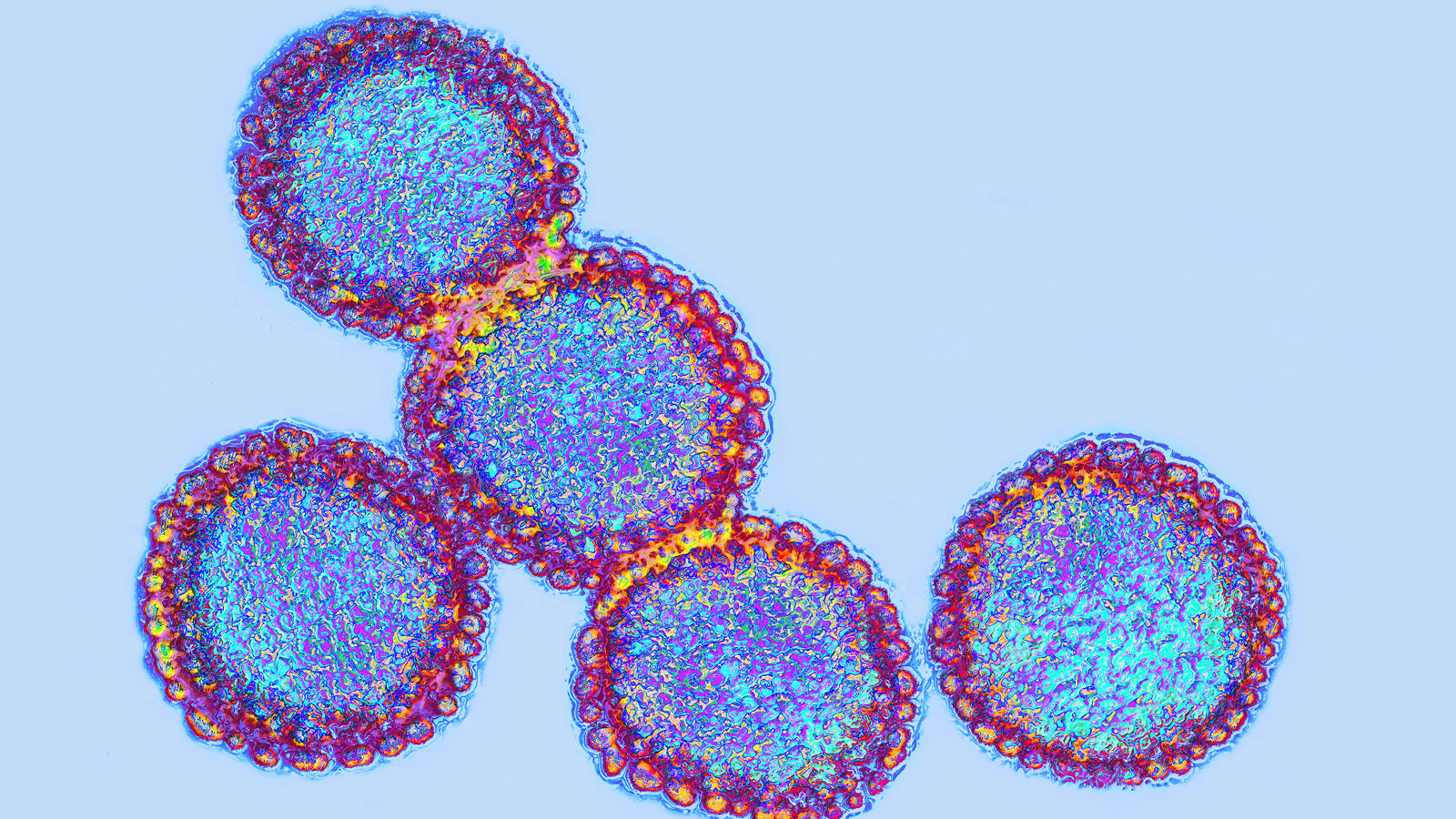
Tuberculosis (TB) is a bacterial infection, often of the lungs, that can be deadly if left untreated. In fact, TB is one of the top 10 causes of death worldwide, and the rising prevalence of drug-resistant TB is a "public health crisis and a health security threat," according to the World Health Organization (WHO).
One of the oldest diseases known to humans, TB was a leading cause of death in the U.S. and Europe in the last century, but advances in living conditions and the introduction of antibiotics has steadily decreased the number of cases in developed countries. In the U.S., the Centers for Disease Control and Prevention (CDC) reported 9,025 cases of TB in 2018 and the agency estimates that up to 13 million Americans live with a form of asymptomatic TB.
A quarter of the world's population is infected with TB bacteria, according to the CDC. However, not everyone infected with the bacterium becomes sick. This is called a latent infection; a person with latent TB doesn't experience symptoms and can't spread the disease to others.
Symptoms of tuberculosis
The incubation period, or the time it takes for symptoms to develop once a person has been infected with TB, varies from a few weeks to many years, according to the CDC.
Common symptoms of an active TB infection include coughing — and coughing up blood or sputum — chest pain, fatigue and night sweats. TB can damage the lungs during an infection, causing inflammation that makes it difficult to breathe. A patient with an active TB infection may also have an abnormal chest X-ray.
Although TB could be mistaken for pneumonia or chronic obstructive pulmonary disease (COPD), the specific symptoms and diagnostic testing make TB a straightforward diagnosis, said Sabine Ehrt, a professor of microbiology and immunology at Weill Cornell Medicine in New York.
A latent infection of TB, on the other hand, does not cause any symptoms, and only diagnostic testing can reveal if an otherwise healthy person has TB. Latent infections can take years to turn into active disease, and some people with latent TB infections never develop the active disease. It's unclear what causes a latent TB infection to become active and why some people never develop the active form, Ehrt said.
TB is characterized by a long-term cold war with the body's immune system, said Nicolas Menzies, an assistant professor of global health at the Harvard T.H. Chan School of Public Health in Boston. A latent infection is a sign that the immune system is keeping the number of TB bacteria in check, Menzies said.
Diagnosing tuberculosis
There are two types of tests commonly used to diagnose TB: a skin test and blood tests.
A health care provider administering the TB skin test — also known as the Mantoux tuberculin skin test, or purified protein derivative test — injects tuberculin, a sterile protein extract from the TB bacterium, into the skin of a person's arm. Within two to three days, the person tested for TB must return to their health care provider, who will look for a positive reaction at the injection site. A reaction might look like a raised, hard or swollen area, and a health care provider may measure the size of the area with a ruler, according to the CDC. A positive reaction means the person has been infected with TB bacteria, but further tests, such as a chest X-ray or physical examination, are needed to distinguish an active infection from a latent one. According to Ehrt, the TB skin test is the most commonly used diagnostic tool in the U.S.
In countries and regions where TB is endemic, such as India, China and Indonesia, blood tests are more successful at diagnosing TB. That's because a person who has received the Bacillus Calmette-Guérin (BCG) vaccine for TB may give a false positive result after a skin test. This vaccine is rarely given in the U.S., according to the National Institutes of Health (NIH), but it is common where TB is prevalent.
A blood test requires blood samples to be sent to a laboratory, where they're exposed to TB bacteria. White blood cells will produce a certain chemical if they've encountered TB before. Like the skin test, blood tests alone cannot determine whether an infection is active or latent.

How is tuberculosis treated?
Active TB infections are treated with multidrug cocktails. The first-line antibiotics prescribed are isoniazid, rifampin, ethambutol and pyrazinamide. This regimen may last six to nine months, according to the CDC.
Patients who do not complete the full regimen may develop multidrug-resistant (MDR) or extensively drug-resistant (XDR) TB infections. MDR-TB is defined as being resistant to at least rifampin and isoniazid, while XDR-TB is resistant to both these first-line drugs and at least two second-line medicines. The WHO estimates that in 2016, 4.1% of new TB cases and 19% of previously treated TB cases were MDR- or rifampin-resistant, and 123 countries to date had reported at least one case of XDR-TB.
MDR or XDR are a result of the antibiotics not wiping out all the TB bacteria, according to a review published in the journal Clinical Infectious Diseases. If bacteria are left at the end of a regimen (which is likely when the regimen isn't completed), then those bacteria have a higher chance of becoming resistant to the drugs made to combat them.
One of the goals of current TB research is to discover new drugs and fine-tune existing therapies to shorten drug regimens, Ehrt said. Even shortening it to two months would be a "big step forward," she said.
Once treatment is complete, the TB bacteria are eliminated from the body. While there is still the possibility of a new infection, most healthy people won't need treatment again, according to the CDC.
Preventing tuberculosis
A century ago, Albert Calmette and Camille Guérin, both researchers at the Pasteur Institute in France, developed a vaccine for TB from weakened strains of the bacterium. Called the BCG vaccine, forms of it are produced today by different manufacturers around the world, but there is controversy around its efficacy.
According to the U.K.'s National Health Service, the BCG vaccine is 70% to 80% effective against the most severe forms of TB including TB meningitis in children, but it's less effective in preventing respiratory TB in adults. The vaccine isn't widely used in the U.S., according to the CDC, but may be administered to children if their families are from places with high rates of TB, if TB was reported in their neighborhood or if they plan to travel to a country with high rates of TB.
One of the WHO's approaches to the prevention of TB is to manage latent TB infections to stop them from progressing to active disease. In 2018, the CDC updated its recommendations for the treatment of latent TB. Once a case of latent TB is diagnosed, a patient may be put on a treatment regimen of isoniazid, rifampin or a combination of isoniazid and rifapentine. The CDC's recommended duration for this treatment depends on the drug used and whether the patient is an adult or a child, but it can last from three to nine months.
TB is known as a disease of poverty, said Menzies, "and for good reason: If someone is infected with TB, they are much more likely to progress to active disease if they are underweight." Other risk factors include being older and having a compromised immune system. According to the NIH, TB is one of the leading causes of death among people with HIV, a disease that weakens the immune system.
Additional resources:
- Learn about respiratory tuberculosis at the American Lung Association.
- Read stories from TB survivors, from the CDC.
- Read about the WHO's End TB strategy.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Flu: Facts about seasonal influenza and bird flu
What is hantavirus? The rare but deadly respiratory illness spread by rodents