What are cytokines?
Cytokines are the unsung heroes of the immune system, often acting as the first responders to a pathogen infection.

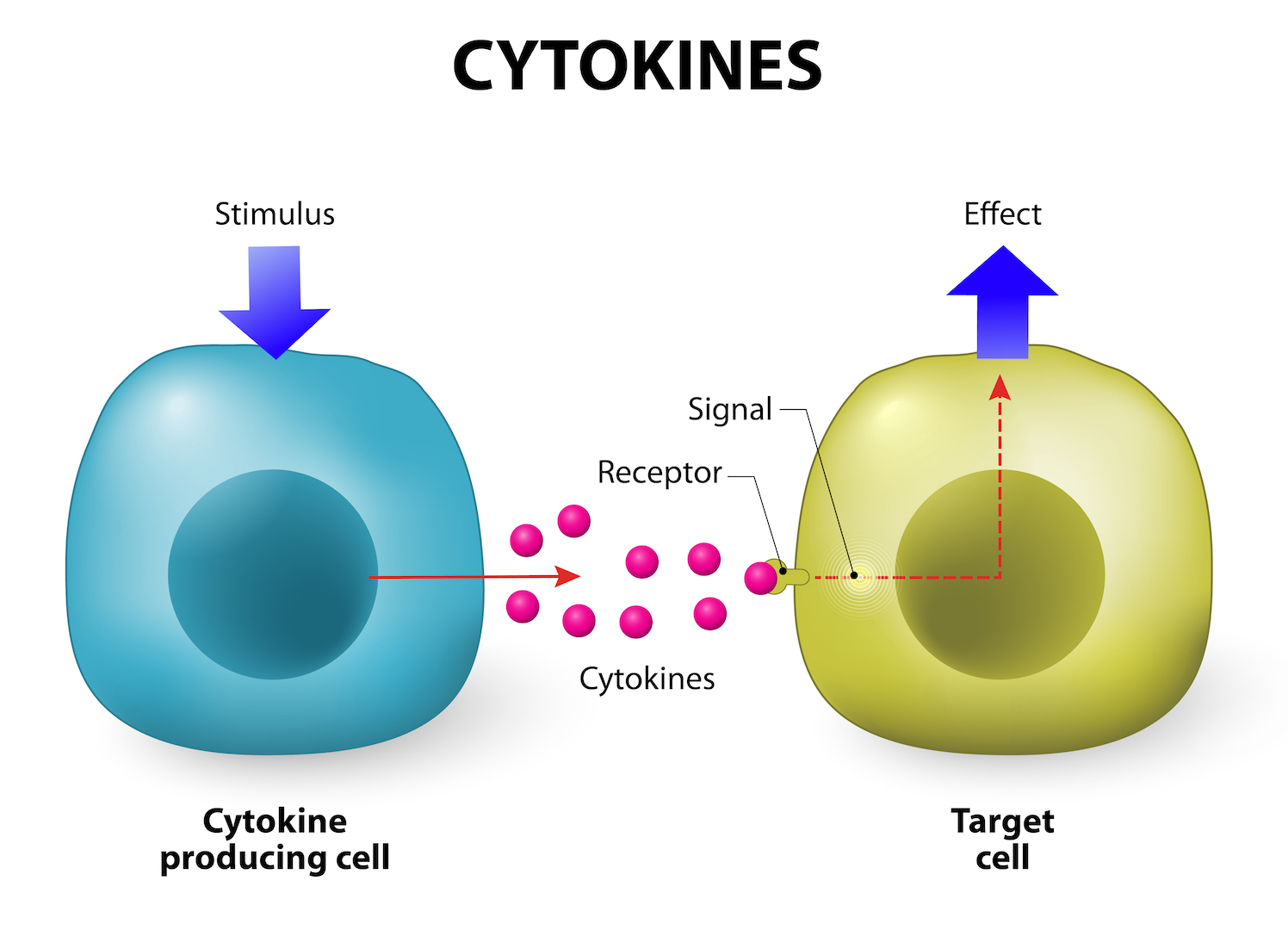
Cytokines are molecules that allow your cells to talk to each other, and are crucial for healthy immune system function. Too many cytokines, however, can have a negative effect and result in what's known as a "cytokine storm."
These small signaling molecules are produced by many different immune cells, such as neutrophils (some of the first cells to travel to an infection site), mast cells (responsible for allergic reactions), macrophages, B-cells and T-cells, according to a 2014 review published in the journal Frontiers in Immunology.
Cytokines radiate out from cells "kind of like a Wi-Fi signal," said Joyce Wu, an immunobiologist at the University of Arizona in Tucson. They then bind to specific receptors on both immune and non-immune cells, and may signal the cell to adjust how it grows or behaves. Nearly every organ of the body contains cells with cytokine receptors.
Chemokines are cytokines that act like a beacon directing immune cells where to go. In this way, chemokines help immune cells find and destroy whatever harmful invader has entered the body.
While cytokines typically come from immune cells, they can also come from non-immune cells, said Mandy Ford, an immunologist at Emory University in Atlanta, Georgia. Endothelial cells, which are the cells lining the inside of blood vessels, and epithelial cells, which are the cells covering the surface of organs, skin and other tissue, can also send cytokines around the body.
How do cytokines work?
When a pathogen, or harmful invader enters the body, immune cells, cytokines and organs respond by working together like an orchestra, Ford said. The first immune cell to notice the pathogen is like the conductor. That cell directs all the other cells by creating and sending out messages (cytokines) to the rest of the organs or cells in the body (the orchestra members), which then respond as directed.
"The initiation of cytokine secretion tells the rest of the immune cells, and also non-immune cells in the body that there is a pathogen present, and an immune response should be occurring," Ford said.
One of the immune responses cytokines may elicit is inflammation. Cytokines help inflame tissue by directing the cell walls of blood vessels to become more porous by reducing cell-to-cell contact, Ford said. Blood vessels will then leak blood into the surrounding tissue, allowing immune cells to travel via the leaked fluid to the damaged area, and start the healing process.
While cytokine production mainly occurs when the body is infected by a pathogen, cytokine-induced inflammatory responses also happen when tissues are physically damaged, such as if you tripped and cut your knee on the sidewalk.
Are cytokines part of the innate or adaptive immune system?
Our immune system can be divided into two categories: the innate immune system and the adaptive immune system. The innate immune system refers to the immunity that you're born with, which targets general health threats, while adaptive immunity refers to acquired immunity, which targets more specific pathogens.
Cytokines are "at the crossroads of bridging the communication between the innate and adaptive immune responses," Ford said. That's because the amount and type of cytokines that cells secrete differ depending on the type of pathogen, and those differences help the immune system appropriately tailor its response to be innate or adaptive. Certain cytokines can stimulate either the innate immune system, adaptive one, or a mix of both depending on the infection.
Cytokines can also direct brain cells to release chemicals that tell your body that you're sick, prompting you to rest and avoid activities that could further expose you to pathogens. "Tiredness, lethargy, malaise and just that kind of achy feeling is the impact of cytokines on our bodies," Ford said.
Related: 11 surprising facts about the immune system
Without cytokines, the innate immune system wouldn't know when to activate because there would be no indication of a threat. Once activated, innate immune cells don't secrete cytokines intended for any specific receptors at first, Ford said. Rather, secreted cytokines will target the entire body, causing fever, achy joints and fatigue, according to a 2007 study published in the journal International Anesthesiology Clinics. The adaptive immune system will eventually secrete specific cytokines that target and activate T-cells in order to fine-tune the immune response toward the specific introduced pathogen, reported a 2010 study from The Journal of Allergy and Clinical Immunology.
Cytokines signal the adaptive immune system to activate when the innate immune system fails to subdue an infection. While the innate immune system is good at warding off general health threats, it may fail to destroy foreign pathogens. Cytokines direct the adaptive immune system to produce pathogen-specific antigens that quickly identify the pathogen so the immune system can destroy it.
The cytokine response is slow, and for good reason, Wu said. A 2020 editorial published in the journal JAMA Internal Medicine describes how a rapid immune response in which loads of cytokines are released would cause hyperinflammation, which can lead to shock and organ damage. The slow initial response of the innate immune system prevents the release of too many cytokines at one time, avoiding collateral damage to the body, according to a 2007 study published in the journal Nature Public Health Emergency Collection. The fine-tuned T-cell response can then attack the infection without causing excess harm to the body.
When are cytokines a bad thing?
Cytokines help your body fight off and kill infections, but too many cytokines overwhelm the body and create what is known as a "cytokine storm." It's a "simple analogy to a weather-type storm where it's too much of a good thing," Ford said.
A cytokine storm may occur when too many pathogens enter the body at once, or if the body secretes the wrong type of cytokine early in the immune response, in which case the excessive cytokines can't accurately direct the immune system to clear out the pathogen. Because nearly every organ has cytokine receptors, almost every part of the body is susceptible to the negative effects of a cytokine storm.
A normal release of cytokines causes blood vessel walls to become leakier in order to promote healing of damaged tissue via inflammation, but too many cytokines may cause blood vessels to become overly porous and result in low blood pressure. That, in turn, depletes organs of oxygen and could eventually cause death, Ford said.
Related: Woman with COVID-19 developed a rare brain condition. Doctors suspect a link.
Patients with sepsis or uncontrolled bacterial infections typically experience a cytokine storm, and it's also a symptom of some diseases, such as COVID-19, as described in the JAMA Internal Medicine editorial. A cytokine storm is essentially an uncontrolled immune response that leads to reduced oxygen in the blood, fluid build-up in the lungs, difficulty breathing, and many of the other symptoms observed in COVID-19 illnesses, Ford said.
Whether induced by COVID-19 or not, cytokine storms can also cause neurological issues. The brain is naturally protected from harmful chemicals thanks to the blood-brain barrier. But cytokines are much smaller than cells, so they can slip through the brain's protective membrane. Cytokine storms have been known to cause symptoms such as headache, migraine, decreased appetite, increased need for sleep and overwhelming fatigue, according to a 2009 review published in the journal Psychiatry.
Treating COVID-19 cytokine storms
Some research suggests that cytokine storms are a major reason for illness and death among COVID-19 patients, according to the JAMA Internal Medicine editorial. A 2020 study published in the journal Clinical Infectious Diseases found the cytokine inhibiting drug tocilizumab has been shown to reduce mortality in COVID-19 patients on ventilators by 45%.
Related: Treatments for COVID-19: Drugs being tested against the coronavirus
Cytokine levels can also influence the care COVID-19 patients receive. The presence and amount of certain cytokines can predict the survivability of COVID-19 cases, reported a recent study published in Nature Medicine. This can help doctors create an effective treatment protocol depending on cytokine severity. Although the mechanisms underpinning the severity of COVID-19 are still poorly understood, a recent review published in the journal Cardiorenal Medicine found that properly timed anti-inflammatory strategies may help reduce the severity of cytokine storms and can improve a patient's health when infected.
Additional resources:
- Here's how doctors and professors at the Yale School of Medicine describe cytokine storms.
- Learn more about how cancer researchers use cytokines as therapy, from the Center for Cancer Research.
- Watch this video explaining the relationship between cytokine storms and COVID-19 severity from the Johns Hopkins Bloomberg School of Public Health.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.










