Will we need more COVID-19 boosters to end the pandemic?
Omicron is a reminder that the pandemic is not over yet.

Omicron's explosive surge in the U.S. is a painful reminder that the pandemic is far from over.
It also raises some questions. Will the pandemic ever end? And will we need more boosters to enter the "endemic" phase of transmission, in which COVID-19 case counts don't break records and hospitals aren't strained?
"I think many of us working in infectious disease realized that after the first couple of surges, it wouldn't just go away completely, because that's not what viruses like this do," Dr. Shruti Gohil, associate medical director of epidemiology and infection prevention at the University of California, Irvine, told Live Science.
Related: 14 coronavirus myths busted by science
The pandemic phase of transmission will end, but to get to an endemic phase faster, we will probably need additional COVID-19 boosters that target different variants and keep the virus from causing large outbreaks, experts told Live Science. Eventually, a yearly or seasonal vaccine may be needed to keep case counts low and to make COVID-19 more of a nuisance than an existential threat — something that, for most people, would be like dealing with the common cold, Gohil said.
A big factor in how long it takes to go from a pandemic to an endemic phase depends on how fast it takes to vaccinate more of the world and more of the U.S. population.
More shots are coming
In a cloudy crystal ball, Dr. Sharon Nachman, chief of the Division of Pediatric Infectious Diseases at Stony Brook Children's Hospital in New York, sees boosters being given once a year. Several studies suggest that initial vaccines wane in effectiveness after about five to six months; protection against infection drops fairly quickly, while the dramatic reduction in hospitalization is more durable. Without yearly boosters, COVID-19 will be less manageable as surges of severe cases strain hospital resources. “But if COVID-19 turned endemic like the flu, we’re all going to get a cold and that’s really it,” Nachman said.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
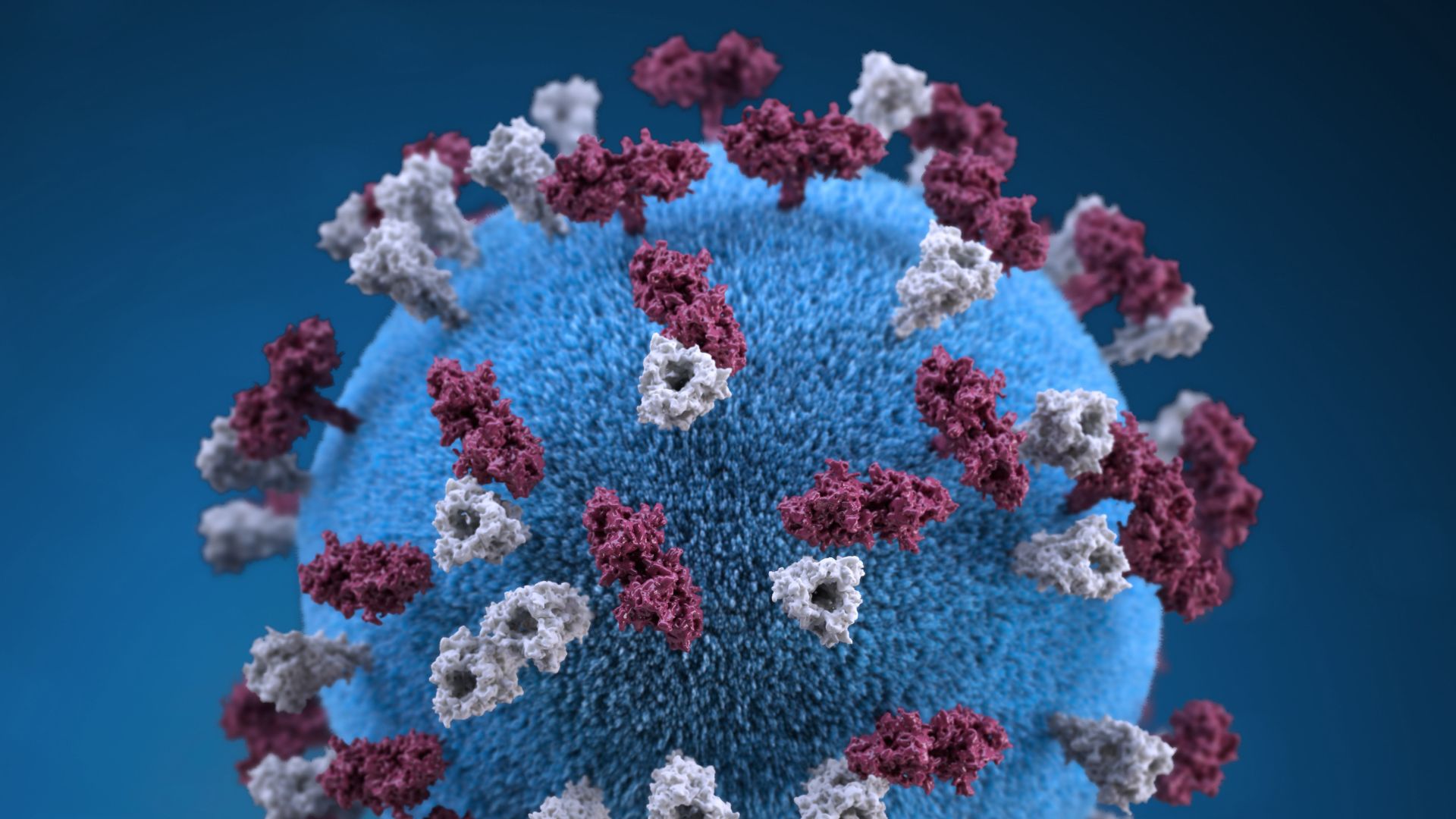
And because SARS-CoV-2 (the virus that causes COVID-19) can mutate into more infectious and/or immune-evading variants, as omicron has clearly shown, we will probably need to update vaccine formulations, Gohil said.
In the more distant future, COVID-19 mRNA vaccines will likely target multiple variants of concern, Gohil said. She compared it to how vaccine makers design the flu vaccine each year to target two to four flu viruses circulating earlier in the year in the Southern Hemisphere, with the goal of stimulating the body to produce a mixture of antibodies that match currently circulating strains of flu.
But in the short term, we may need boosters targeting a specific variant. Vaccine manufacturers such as Pfizer-BioNTech and Moderna are working on creating omicron-specific boosters, according to Reuters. However, using variant-specific boosters is likely a temporary measure, Nachman said. Over time, she said, companies should develop and produce vaccines that stimulate an immune response to many different versions of the SARS-CoV-2 spike protein, which the virus uses to latch onto and infect cells.
"I think our boosters will contain spike-protein sequencing from around the world so that when those viruses do change or they get close to us, we'll have cross-variant protection," Nachman told Live Science. Having one vaccine that induces cross-protective immunity would mean you'd get one vaccine a year rather than, say, four variant-specific ones.
Vaccinating everyone is key
Reaching an endemic stage would mean the virus is circulating at low but steady levels. In that scenario, there are predictable patterns of infection, there are no record-breaking case counts and hospitals are not overwhelmed with surges of severe infections.
However, endemicity will be elusive until there are higher rates of global vaccination, says Dr. Erica N. Johnson, chair of the Infectious Disease Board for the American Board of Internal Medicine and an assistant professor of medicine at the Johns Hopkins University School of Medicine. “There are a lot of places in the world that don't have the same vaccine availability. Until we solve that problem, I don't think we're going to get to a place where this becomes just another endemic virus.”
Global access to vaccines is important because variants are fueled by the virus spreading and replicating, which occurs more easily in unvaccinated people or people who are immunocompromised.
That means getting more of the population vaccinated is key to reaching endemicity. While past infection does provide immunity against infection — one study found immunity from a prior infection led to a 50% decrease in the risk of hospitalization— that protection is fleeting and variable and works less well to prevent hospitalization, Live Science previously reported. A CDC study found that compared to vaccinated individuals, unvaccinated individuals who recovered from a past infection were 5.49-fold times more likely to get COVID-19 illness.
For people who are unvaccinated, COVID-19 will be an ongoing concern, Nachman said. "We're seeing that now as [unvaccinated people] who had coronavirus earlier are getting sick again," Nachman said. "And we're seeing them sicker than those who got a COVID-19 vaccine after having a prior illness."
In the future, SARS-CoV-2 will join a host of other viruses, such as respiratory syncytial virus (RSV) and influenza, that regularly circulate but do not upend daily life.
Moreover, there are now antivirals that can prevent severe disease if they are taken in the first few days of COVID-19 infection. Early data published to the preprint database bioRxiv found the current antivirals were effective against omicron.
COVID-19 is here to stay, but it will eventually become a more manageable threat. To keep it that way, we may be looking at a future of annual boosters.
Originally published on Live Science.

Jocelyn is a New York-based science journalist whose work has appeared in Discover Magazine, Inverse and Verywell Health, among other publications. She holds a master's of Psychology with a concentration in behavioral neuroscience and a bachelor's of science in integrative neuroscience from Binghamton University. She has reported on several health and science topics ranging from coronavirus news to the latest findings in gut health.